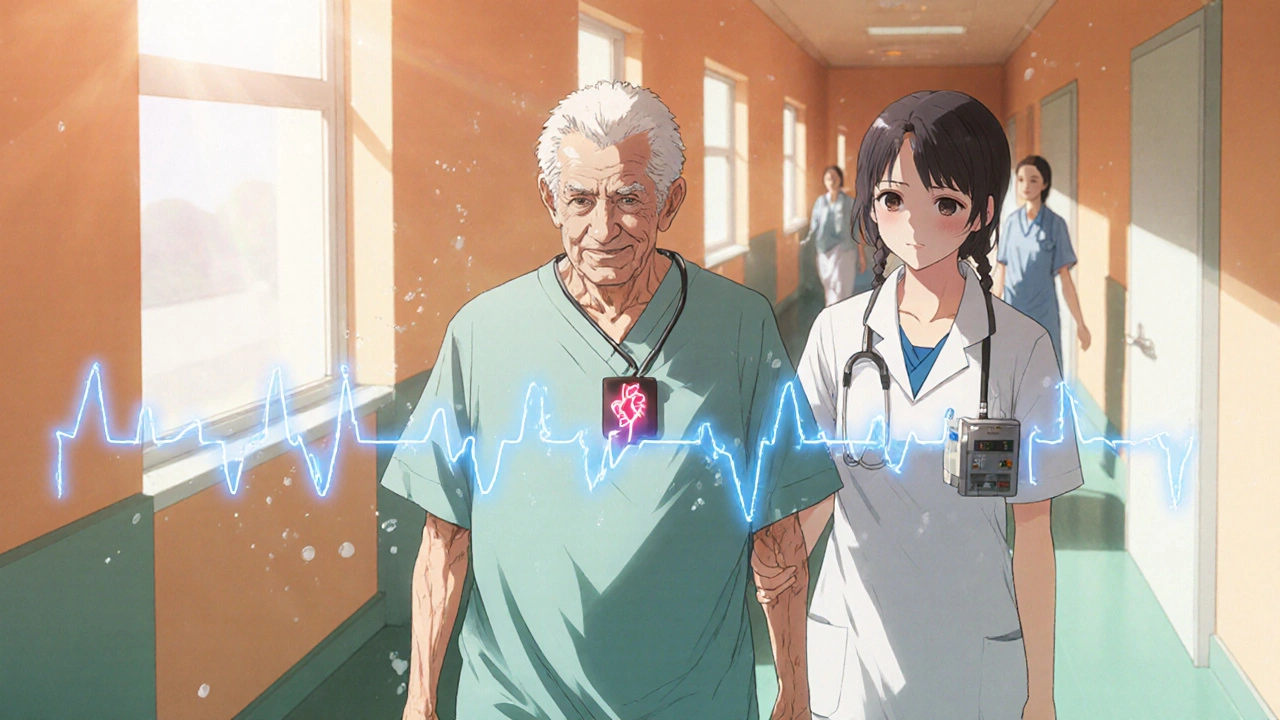
Safe Heart Exercise: What Works, What to Avoid, and How to Stay Protected
When you have heart disease, are on heart medication, or are recovering from a heart event, safe heart exercise, physical activity tailored to protect and strengthen the heart without triggering danger isn’t just a good idea—it’s a necessity. But it’s not about pushing harder. It’s about knowing your limits, understanding how your meds affect your body, and moving in ways that support healing, not stress. Many people think exercise means running or lifting heavy weights, but for heart health, it’s often walking, cycling, or light resistance training done at the right pace and monitored closely.
Cardiac rehabilitation, a structured program that guides people with heart conditions through safe physical activity and lifestyle changes is the gold standard for starting out. It’s not just for people after a heart attack—it’s for anyone on heart medication, drugs like beta blockers, calcium channel blockers, or diuretics that change how your heart responds to effort. These meds can lower your heart rate, reduce blood pressure, or alter your body’s ability to sweat or feel fatigue. That means your usual sense of exertion? It might be wrong. You might not feel your heart racing even when it’s working too hard. That’s why safe heart exercise isn’t guesswork. It’s measured, often with a doctor’s input, and sometimes with a wearable monitor.
What you avoid matters as much as what you do. Heavy lifting, sudden sprints, or exercising in extreme heat can be risky if your heart isn’t ready. Even some herbal supplements—like Arjuna bark extract, a natural heart support supplement sometimes used alongside conventional treatment—can interact with your meds and change how your body handles exertion. That’s why the posts below cover everything from comparing heart meds like Diltiazem and Labetalol, to how Indapamide affects fluid balance during activity, and why knowing your exact medication profile is the first step to safe movement.
You’ll find real guidance here—not theory. People who’ve been through it share how they adjusted their walks after a stent, how they timed their exercise around pills, and what signs told them to stop. You’ll see how medication synchronization helps avoid missed doses that could throw off your rhythm during a workout. You’ll learn why checking FDA alerts matters if your heart meds get recalled or updated. And you’ll understand how tools like Tiova Rotacap or Besivance don’t just treat lung or eye issues—they can indirectly affect your energy and breathing during exercise.
There’s no one-size-fits-all plan. But there is a clear path: know your body, know your meds, and move smart. The posts ahead give you the tools to do exactly that—without the fluff, without the fear, and without the guesswork.