After a heart attack, bypass surgery, or other major cardiac event, the last thing you want to do is push yourself too hard. But doing nothing can be just as dangerous. The truth is, exercise is one of the most powerful tools you have to rebuild your heart health - if you do it right. Thousands of people recover fully after heart events, not because they were lucky, but because they followed a structured, safe plan. This isn’t about getting back to the gym or running marathons. It’s about slowly, steadily, and safely rebuilding strength, stamina, and confidence - one step at a time.
Why Exercise After a Heart Event Isn’t Optional
Many people think rest is the best medicine after a heart problem. But research shows the opposite. People who start moving again under medical supervision cut their risk of another heart event by 20-30%. They’re 47% less likely to be readmitted to the hospital within a year. And their chances of living five more years improve by 30% compared to those who stay inactive.
This isn’t guesswork. It’s science. Cardiac rehabilitation programs - supervised, personalized, and evidence-based - have been proven to work. They don’t just help your heart. They reduce anxiety, improve sleep, lower blood pressure, and help you feel like yourself again. The American Heart Association gives cardiac rehab the highest evidence rating: strong, consistent, life-saving results.
The Three Phases of Safe Recovery
Recovery isn’t one-size-fits-all. It happens in clear stages, each with its own goals and limits. Skipping ahead can be risky. Going too slow can delay progress. Here’s what each phase looks like in real life.
Phase 1: In the Hospital - Gentle Movement Begins
Within 24 hours after a stable heart event, you’re encouraged to sit up, swing your legs over the side of the bed, and take a few steps. Sounds simple? It is - and that’s the point.
Exercises here are tiny: ankle pumps while lying down, seated marching (10-15 reps per leg), and short walks down the hallway. These movements keep blood flowing, prevent clots, and stop muscles from stiffening. You won’t break a sweat. Your heart rate might only go up 10-15 beats above resting. That’s normal.
Doctors use something called METs (metabolic equivalents) to measure effort. In this phase, you’re working at 1-2 METs. For reference, sitting quietly is 1 MET. Walking slowly is 2 METs. You’re not pushing. You’re waking your body up.
Phase 2: After Discharge - Building Confidence
Once you’re home, you’ll likely enter a formal cardiac rehab program. This is where real progress begins. Most programs run 3-6 months, with sessions two to three times a week.
Exercise starts with walking. Five to ten minutes a day. That’s it. You’ll increase by a minute or two each session. Within four to six weeks, you’re aiming for 30 minutes a day, five days a week.
Your heart rate target? Resting heart rate + 20-30 beats per minute. If your resting rate is 70, aim for 90-100 during exercise. You’ll wear a monitor to track it. But you don’t need to stare at numbers. Use the talk test: if you can speak in full sentences without gasping, you’re in the right zone.
Don’t skip strength training. Light resistance bands or 1-2 lb weights, two days a week, help you carry groceries, climb stairs, and get out of chairs without help. You’re not lifting heavy. You’re building endurance and balance.
Phase 3: Long-Term Maintenance - Living Strong
After completing rehab, your goal is to keep going - on your own. The American Heart Association recommends at least 150 minutes of moderate aerobic activity per week. That’s 30 minutes, five days a week. Or 75 minutes of brisk walking, cycling, or swimming.
Plus, muscle-strengthening activities twice a week. You can use resistance bands, dumbbells, or bodyweight moves like seated leg lifts or wall push-ups.
Intensity matters. You should be able to talk but not sing. If you’re out of breath after two sentences, you’re going too hard. Your heart rate should stay under your maximum target (usually 85% of your age-predicted max - but your doctor will give you your personal number).
What to Avoid - Red Flags That Mean Stop
Exercise is safe - but only if you listen to your body. Some symptoms are normal. Others are warnings. Know the difference.
Stop immediately and call your doctor if you feel:
- Chest pain, pressure, or tightness
- Pain spreading to your arm, neck, jaw, or back
- Dizziness or lightheadedness
- Unusual shortness of breath (not from being out of shape)
- Palpitations - your heart skipping, racing, or fluttering
- Sudden weakness or numbness on one side
- Slurred speech or confusion
These aren’t just "bad days." They’re signals your heart is under stress. Don’t ignore them. Don’t push through. Call your care team. Better safe than sorry.

Supervised Rehab vs. Going It Alone
You might think: "I can just walk on my own. Why go to rehab?" The numbers say otherwise.
People in formal cardiac rehab programs recover 25% faster and have 30% lower five-year death rates than those who exercise alone. Why? Because rehab isn’t just about exercise. It’s about education, monitoring, and support.
Without supervision, 27% of people push past safe heart rate limits within the first month. Some don’t realize their meds (like beta-blockers) lower their max heart rate by 20-30%. They think they’re not working hard enough - so they push harder. That’s dangerous.
Rehab programs also teach you how to track your own symptoms. They help you build a routine that fits your life - not the other way around. And they’re there if something goes wrong.
That said, if you’re low-risk, have a strong support system, and your doctor clears you, self-directed exercise can work - after you’ve completed at least 6-8 supervised sessions.
Barriers and Real Solutions
Only 20-30% of eligible patients in the U.S. enroll in cardiac rehab. Why? Transportation. Work schedules. Insurance confusion. Fear.
But solutions are here.
Transportation? Many programs offer shuttle services. Others partner with ride-share apps.
Work conflicts? Hybrid programs now exist. You do 12 sessions in person and 24 online, using a Bluetooth heart rate monitor and video check-ins. One study showed 89% adherence with this model.
Cost? Medicare and most private insurers cover 36 sessions after a qualifying event. Check your policy - you’re likely covered.
Anxiety? It’s common. 68% of patients fear another heart attack when they move. But after four weeks in rehab, 82% say their fear drops dramatically. You’re not alone. The staff has seen it before - and they know how to help.
New Trends - What’s Changing in 2025
Cardiac rehab isn’t stuck in the past. Here’s what’s new:
- HIIT is now safe - High-intensity interval training (short bursts of harder effort) is proven safe and effective for stable patients. It improves fitness 37% more than steady walking.
- Wearables are standard - Most accredited programs now use FDA-cleared smart patches and heart rate monitors that send data to your care team in real time.
- AI is stepping in - Mayo Clinic is testing algorithms that adjust your workout intensity based on your real-time heart rate, breathing, and sleep data. Early results show 28% better adherence.
- Earlier movement - Low-risk patients are now encouraged to walk within 24 hours after a procedure, not 48. Recovery starts faster.
These aren’t futuristic ideas. They’re happening now. And they’re making rehab more effective - and more accessible.
What Success Looks Like
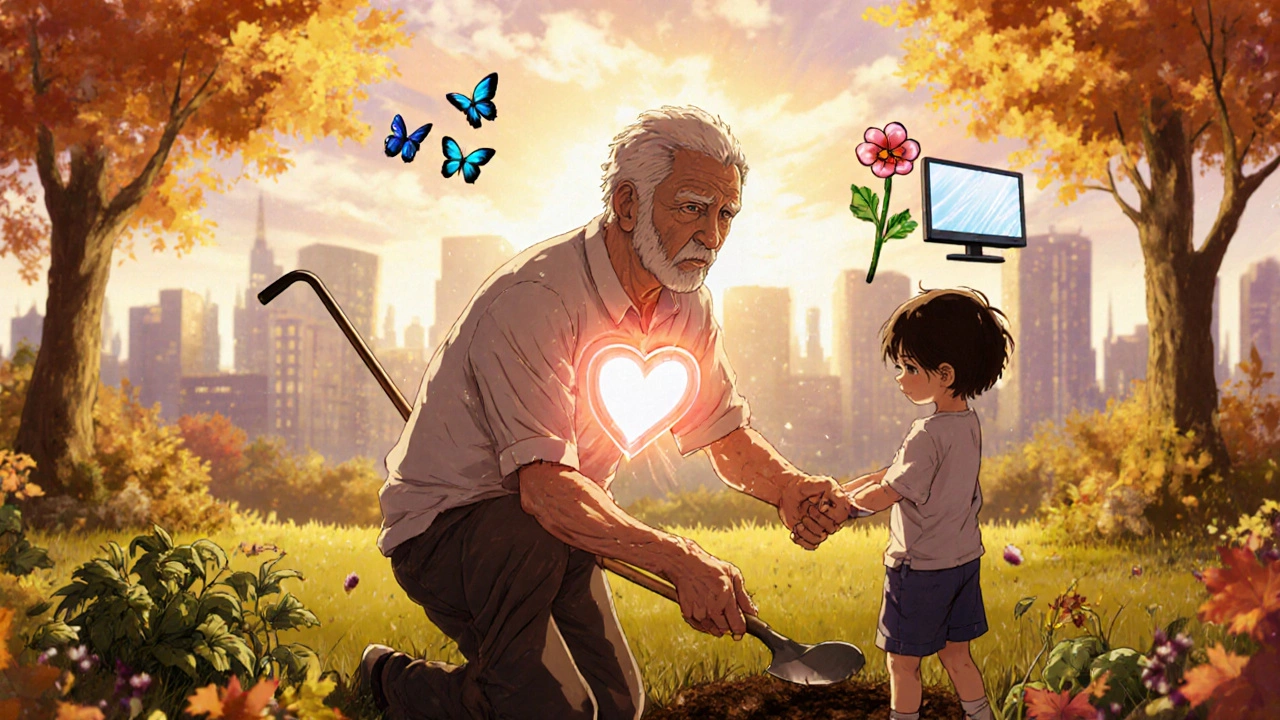
One 68-year-old man from Birmingham, after a heart attack in January 2024, started rehab in February. He could barely walk to the mailbox. By week 12, he was walking 30 minutes daily. By six months, he was gardening again, carrying his grandson, and sleeping through the night.
He didn’t run a 5K. He didn’t lift weights like a bodybuilder. He just kept showing up. He learned his limits. He trusted the process.
That’s what recovery looks like. Not perfection. Not speed. Consistency.
Getting Started - Your Action Plan
If you’ve had a heart event, here’s what to do next:
- Ask your doctor for a referral to cardiac rehab. Don’t wait. Don’t assume you’ll get one automatically.
- Get your baseline - A stress test or six-minute walk test will help set your safe heart rate zone.
- Start slow - Walk 5-10 minutes. Do ankle pumps. Sit and stand from a chair. No rush.
- Track your symptoms - Keep a simple journal: date, activity, how you felt, heart rate (if you have a monitor).
- Use the talk test - If you can’t talk without gasping, slow down.
- Stick with it - The first month is the hardest. The payoff comes after 6-8 weeks.
You don’t need to be perfect. You just need to be consistent. Your heart isn’t broken. It’s healing. And it needs movement to do it right.
Can I exercise right after being discharged from the hospital?
Yes - but only gentle movement. Most patients are encouraged to sit up, walk a few steps, and do ankle pumps within 24 hours after a stable heart event. This helps prevent blood clots and muscle stiffness. Always follow your care team’s instructions. Don’t push yourself. Even walking to the bathroom counts as progress.
How do I know if I’m exercising too hard?
Use the talk test: if you can’t speak in full sentences without gasping, you’re going too hard. Also watch for chest pain, dizziness, unusual shortness of breath, or a heart rate that spikes beyond your target zone (usually resting heart rate + 20-30 bpm). If you feel any of these, stop and rest. If symptoms don’t go away in a few minutes, call your doctor.
Are heart rate monitors necessary for cardiac rehab?
They’re not mandatory, but they’re highly recommended - especially early on. Your target heart rate is personalized and often lower than what’s healthy for someone without heart disease. A monitor helps you stay in the safe zone. Many rehab programs provide Bluetooth monitors that sync with apps and send data to your care team.
Can I do strength training after a heart event?
Yes - but start light. Use resistance bands or 1-2 pound dumbbells. Focus on control, not weight. Do exercises like seated rows, leg lifts, or wall push-ups. Two days a week is enough. Avoid holding your breath or straining. If you feel chest pressure or dizziness, stop immediately.
Does insurance cover cardiac rehabilitation?
Yes - Medicare and most private insurers cover up to 36 sessions after a qualifying heart event like a heart attack, bypass surgery, or stent placement. Some plans also cover telehealth rehab sessions. Check with your provider or ask your doctor’s office to verify coverage before starting.
What if I live in a rural area and can’t get to a rehab center?
Hybrid programs are now widely available. You’ll do 12 in-person visits and 24 virtual sessions using a wearable heart rate monitor and video calls. Many programs mail you the equipment. Studies show 89% of patients stick with these programs. Ask your doctor about telehealth cardiac rehab options in your area.
How long does it take to feel normal again?
Most people notice real improvements in energy, mood, and confidence after 4-6 weeks of consistent rehab. Full recovery takes 3-6 months. It’s not about getting back to how you were before - it’s about building a healthier, stronger version of yourself. Progress isn’t always fast, but it’s steady.
Can I return to sex after a heart event?
Yes - for most people, sex is safe after a few weeks of recovery, once you can walk up two flights of stairs without symptoms. It’s similar in intensity to climbing stairs or brisk walking. If you’re unsure, ask your doctor. Many rehab programs include counseling on resuming intimacy safely.
What Comes Next?
Cardiac rehab isn’t the end of your journey. It’s the foundation. Once you’ve built your strength and confidence, you’ll keep exercising - not because you have to, but because you want to. Because you feel better. Because you’re alive.
You don’t need to be an athlete. You just need to move - safely, regularly, and with awareness. Your heart has been through a lot. Now it’s your turn to take care of it - one step, one breath, one day at a time.