When you stand up too fast and feel like the room is spinning, or you turn your head and suddenly get nauseous, you’re not just being clumsy. You might be experiencing vertigo-a specific kind of dizziness where everything feels like it’s moving, even when you’re perfectly still. It’s not the same as feeling lightheaded or faint. That’s dizziness. Vertigo is your inner ear screaming that something’s wrong with your balance system.
What’s Really Going On Inside Your Ear?
Your inner ear isn’t just for hearing. It’s your body’s gyroscope. Inside each ear, there are three fluid-filled loops called semicircular canals, and tiny calcium crystals called otoconia that sit on a gel-like membrane. These crystals help your brain detect head movement-tilting, turning, looking up or down. When they’re in the right place, you stay balanced. When they get loose? Trouble starts. The most common cause of vertigo is benign paroxysmal positional vertigo (BPPV). It happens when those crystals break free and float into one of the canals. Every time you move your head in a certain way-rolling over in bed, looking up at a shelf, bending down to tie your shoes-the crystals shift, sending false signals to your brain. Your brain thinks you’re spinning, even though you’re not. BPPV causes short bursts of spinning, usually 5 to 30 seconds long. It’s harmless but terrifying. About 20-30% of all dizziness cases are BPPV, and over half of dizziness in people over 65 is due to this. Then there’s vestibular neuritis, often triggered by a virus. It inflames the nerve that connects your inner ear to your brain. This doesn’t cause hearing loss, but it can make you feel like you’re on a rocking boat for days or even weeks. You might be too dizzy to walk, eat, or even open your eyes. It’s not dangerous on its own, but it’s exhausting. Another big one is Ménière’s disease. This isn’t just about vertigo. It comes with ringing in the ear (tinnitus), a feeling of fullness or pressure, and fluctuating hearing loss. It’s caused by too much fluid building up in the inner ear. In the U.S., around 615,000 people have it. Attacks can last from 20 minutes to a full day. After an attack, you might feel drained for hours. And then there’s the sneaky one: vestibular migraine. You don’t need a headache to have it. Just vertigo that lasts minutes to hours, often with light sensitivity, nausea, or brain fog. It’s the second most common cause of vertigo after BPPV-and it’s often missed because doctors think it’s just a migraine without the pain.How Do You Know What’s Causing It?
Not all dizziness is the same. That’s why testing matters. A simple test called the Dix-Hallpike maneuver can diagnose BPPV in seconds. Your doctor sits you up, then quickly lays you back with your head turned and hanging slightly over the edge of the table. If you start spinning and your eyes jerk in a specific pattern, you’ve got BPPV. This test is 79% accurate. For more complex cases, especially if vertigo lasts more than a few days or comes with other symptoms like double vision, slurred speech, or weakness, doctors use the HINTS exam. It checks eye movements, head movement response, and whether your eyes are aligned. Done within 48 hours of symptoms, it’s 96.8% accurate at spotting a stroke-something that used to require expensive scans. That’s why emergency rooms now use it as a first step. Blood tests and MRIs aren’t always needed. Most vertigo comes from the inner ear. But if your symptoms don’t match BPPV, neuritis, or Ménière’s, your doctor will look for other causes-like tumors, multiple sclerosis, or even side effects from medications.What Actually Helps? The Real Treatments
Many people reach for pills first-meclizine (Antivert), dimenhydrinate (Dramamine), or promethazine. They work. They make you less dizzy. But here’s the catch: they don’t fix the problem. They just numb your brain’s response. And if you take them too long, your brain stops learning how to compensate. That delays recovery by weeks. The real fix? Movement. Specifically, the right kind of movement. For BPPV, the Epley maneuver is the gold standard. It’s a series of head positions designed to guide the loose crystals back into the right spot. Done correctly, it works in 80-90% of cases after one or two tries. You can do it at home with a video guide, but many people mess it up-wrong angle, not holding the position long enough. That’s why a physical therapist can make the difference between a quick fix and a frustrating repeat. For Ménière’s disease, the answer isn’t surgery right away. It’s salt. Seriously. A daily sodium intake of 1,500 to 2,000 mg cuts vertigo attacks in half for 60-80% of people. That means no canned soup, no processed snacks, no soy sauce. It’s hard. But it works better than most drugs. For vestibular migraine, it’s about prevention. Medications like propranolol or verapamil reduce attacks by 50% in 60% of patients. Keeping a headache diary helps identify triggers-stress, certain foods, lack of sleep. Many patients find that cutting out caffeine or alcohol helps.
Vestibular Therapy: The Quiet Hero
This is where things get powerful. Vestibular rehabilitation therapy (VRT) isn’t magic. It’s science. It’s your brain relearning how to trust your inner ear again. A physical therapist designs exercises tailored to your problem. If you’re dizzy when you look up, you’ll do gaze stabilization exercises. If you’re unsteady walking, you’ll practice balance on uneven surfaces. If you get sick in crowds, you’ll gradually expose yourself to busy environments. The exercises are simple: stare at a finger while moving your head side to side. Stand on one foot with eyes closed. Walk heel-to-toe. Do them twice a day. For 6 to 8 weeks. It’s not fun. In the first week, you might feel worse. That’s normal. Your brain is rewiring. But 70-80% of people see major improvement within a month. And unlike pills, the results last. Your brain doesn’t forget how to balance. The problem? Most people quit. They get discouraged because it’s hard. Or they think, “I’ll do it tomorrow.” But if you stick with it, your chances of recovery jump from 40% to over 90%.What Doesn’t Work (And Why)
There’s a lot of misinformation out there. You’ll hear about essential oils, acupuncture, or “ear crystals” you can buy online. None of these fix BPPV. You can’t massage crystals back into place. And you can’t fix a nerve inflammation with turmeric. Also, don’t avoid movement. Some people stay in bed for days because they’re scared of getting dizzy. That makes it worse. Your brain needs input to heal. Movement-even slow, controlled movement-is medicine. And don’t rely on meds long-term. Meclizine might help you get through a bad day, but if you use it for more than 72 hours, you’re slowing down your natural recovery. Your brain needs to feel the dizziness to adapt to it.When to See a Specialist
If your dizziness lasts more than a few days, comes with hearing loss, vision changes, or weakness, see an ENT (ear, nose, throat doctor) or vestibular specialist. If you’ve had multiple misdiagnoses-“It’s anxiety,” “It’s just aging”-it’s time to push for testing. BPPV is the most commonly missed diagnosis in primary care. One study found half of BPPV cases are misdiagnosed. If your doctor doesn’t do the Dix-Hallpike test, ask for it. It’s free, fast, and accurate. For Ménière’s, if diet and meds aren’t working, there are surgical options. Endoscopic vestibular neurectomy cuts the balance nerve on the affected side. It controls vertigo in 90% of cases and has less than a 5% risk of facial nerve damage.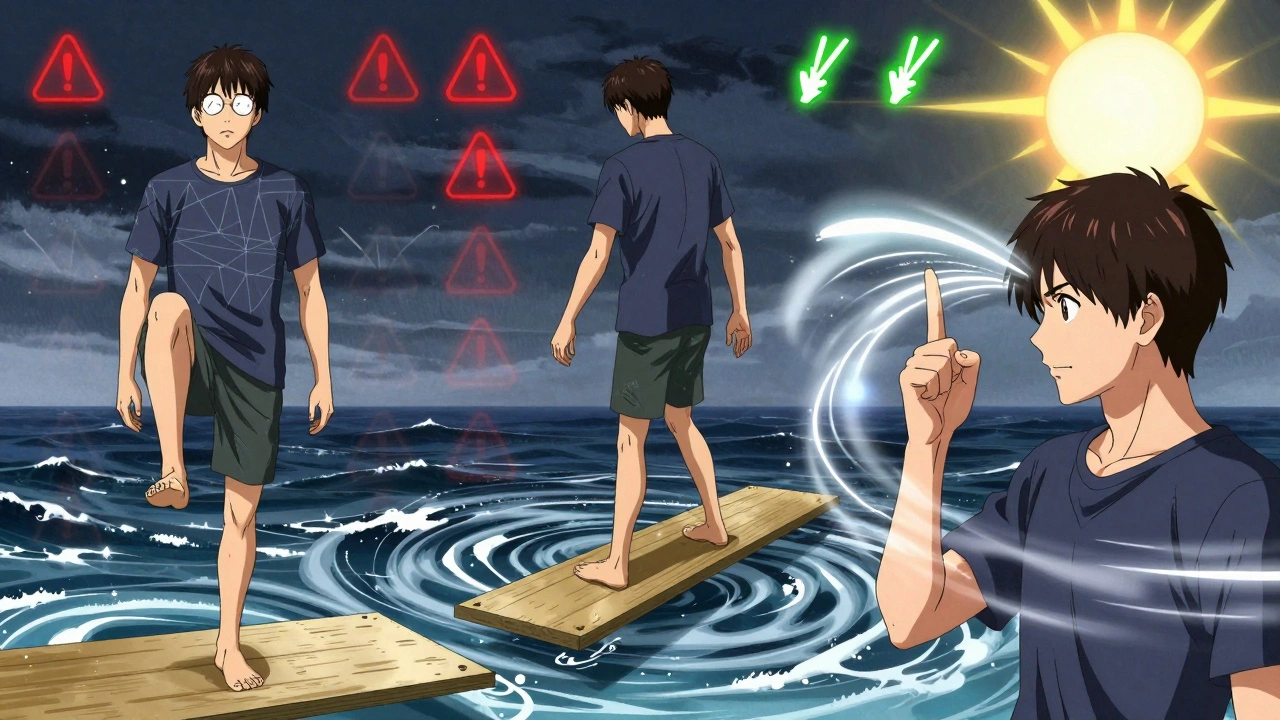
What’s Next for Vertigo Treatment?
Technology is changing how we diagnose and treat vertigo. Smartphone apps like VEDA and VertiGo can now detect abnormal eye movements with your phone’s camera. They’re not perfect, but they’re getting close-85% accuracy in spotting BPPV. That means you might be able to screen yourself at home before ever seeing a doctor. New drugs are coming too. Eptinezumab (Vyepti), approved in 2020, is the first medication specifically for vestibular migraine. It’s an injection given every three months. Early results show 50% fewer vertigo attacks. Researchers are also testing drugs that stabilize the inner ear crystals. One, called CPP-115, reduced BPPV recurrence by 40% in early trials. If it works, it could mean fewer repeat episodes for millions. And insurance? Medicare covers 80% of vestibular rehab. Private insurers usually cover 70%, but often limit you to 10-20 sessions. If you’re not getting enough, ask your therapist to appeal. Many patients get extra sessions approved with a letter from their doctor.Real Stories, Real Results
One woman in Ohio spent three months being told her vertigo was stress-related. She couldn’t work. She stopped driving. Then her physical therapist did the Dix-Hallpike test. BPPV. One Epley maneuver. She was dizzy for 10 seconds. Then she stood up. And the room didn’t spin. She cried. A man in Florida with Ménière’s cut his salt intake to 1,500 mg a day. He stopped eating packaged foods. He cooked everything from scratch. His attacks dropped from daily to once a month. He didn’t need surgery. A college student with vestibular migraine kept a daily log of what she ate, how much she slept, and how her head felt. Within two weeks, she saw a pattern: red wine and skipping meals triggered her. She changed her habits. No more meds. No more missed classes.What You Can Do Today
If you’re dizzy:- Don’t panic. Most causes are treatable.
- Write down when it happens, how long it lasts, and what you were doing.
- Ask your doctor: “Could this be BPPV? Can you do the Dix-Hallpike test?”
- If you’re diagnosed with BPPV, ask for a video of the Epley maneuver. Do it daily for 3 days.
- If it’s not BPPV, ask about vestibular rehab. It’s not optional-it’s essential.
- If you have Ménière’s, start tracking your sodium. Use a food scale. It’s harder than you think.
- Stop taking dizziness pills after 72 hours. Let your brain heal.


