Blood Pressure Estimator
Indapamide Blood Pressure Reduction Calculator
Estimate how much your blood pressure may decrease with Indapamide treatment based on clinical studies showing typical reductions of 8-12 mm Hg systolic and 5-8 mm Hg diastolic in treatment-naïve patients.
Indapamide is a thiazide‑like diuretic used to treat hypertension and edema. It belongs to the class of low‑dose diuretics that combine a powerful natriuretic effect with vasodilatory properties. When doctors prescribe it, the goal is to reduce excess fluid and lower arterial pressure without triggering the sharp electrolyte shifts seen with older thiazides. Indapamide does this through two main pathways - blocking sodium reabsorption in the kidney and relaxing blood‑vessel smooth muscle.
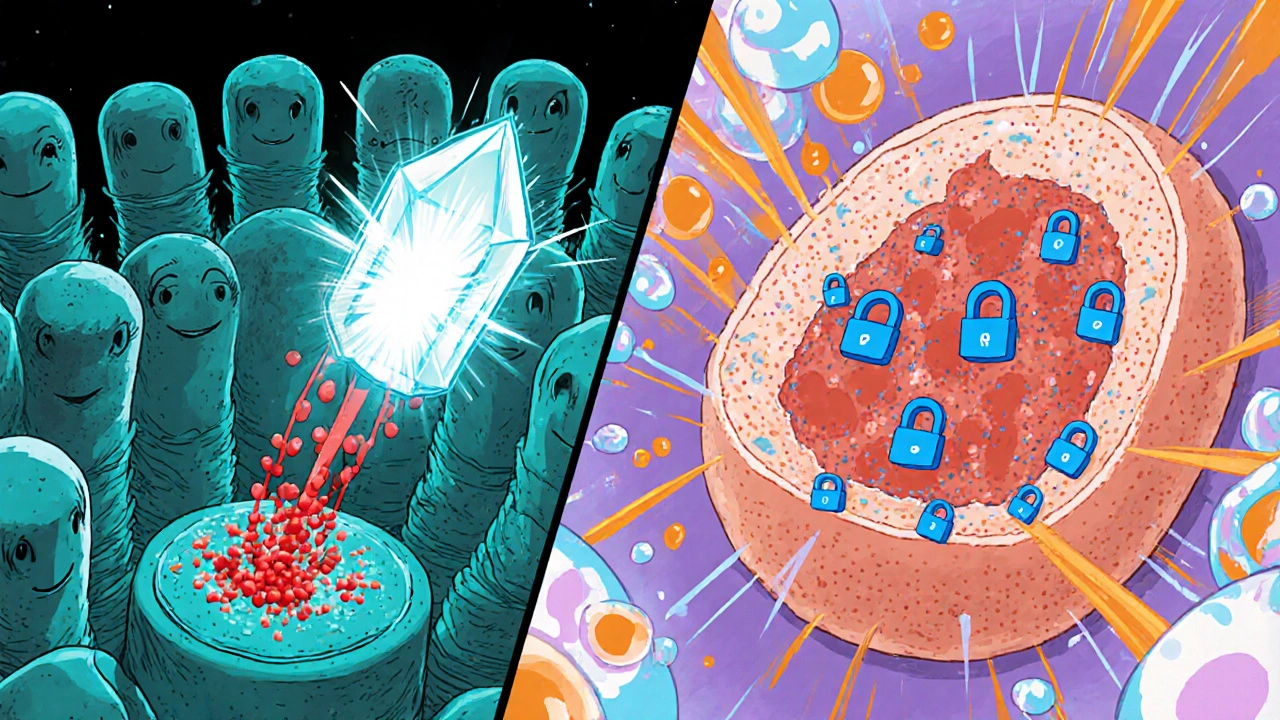
Where Indapamide Hits the Kidney
First, let’s look at the renal side. The drug’s primary target is the Sodium‑Chloride Symporter (the protein that swaps sodium for chloride in the distal convoluted tubule). By inhibiting this transporter, Indapamide prevents the kidney from pulling sodium back into the bloodstream. Less sodium means less water follows, so urine volume rises and blood‑volume drops.
That action takes place in the Distal Convoluted Tubule (the segment of the nephron where fine‑tuning of electrolyte balance occurs). Compared with classic thiazides, Indapamide is a bit gentler on potassium, which translates into fewer cramps and less risk of low‑potassium arrhythmias.
Vasodilation - The Secret Sauce
What sets Indapamide apart is its ability to widen blood vessels. The drug subtly blocks Calcium Channels (pathways that let calcium into smooth‑muscle cells, triggering contraction). Less calcium inside the muscle cells means the arterial walls stay relaxed.
In addition, Indapamide boosts the production of Nitric Oxide (a natural vasodilator released by endothelial cells). The combined effect-less calcium‑driven contraction and more nitric‑oxide‑driven relaxation-lowers peripheral resistance, a key factor in hypertension.
How These Actions Translate to Blood‑Pressure Control
By cutting sodium reabsorption, Indapamide reduces extracellular fluid volume, which directly lowers cardiac output. The vasodilatory component drops systemic vascular resistance. Together, they produce a steady, modest drop in systolic and diastolic pressure, typically 8‑12 mm Hg for systolic and 5‑8 mm Hg for diastolic in treatment‑naïve patients.
Because the fluid‑loss effect is milder than high‑dose thiazides, patients often experience fewer trips to the bathroom at night and less dizziness from sudden volume depletion. This makes Indapamide a popular first‑line option for older adults who need gentle control.
Pharmacokinetics at a Glance
- Absorption: Complete, peak plasma levels in 2-3 hours.
- Half‑life: Approximately 14 hours, allowing once‑daily dosing.
- Metabolism: Minimal hepatic metabolism; primarily excreted unchanged in urine.
- Protein binding: About 60 %.
These properties explain why the drug maintains steady blood levels over a 24‑hour period, supporting consistent blood‑pressure control without the need for multiple daily doses.
Indapamide vs. Hydrochlorothiazide: A Quick Comparison
| Feature | Indapamide | Hydrochlorothiazide (HCTZ) |
|---|---|---|
| Class | Thiazide‑like diuretic | Thiazide diuretic |
| Typical dose | 1.5 mg once daily | 12.5-25 mg once daily |
| Half‑life | ≈14 h | 6-15 h |
| Potassium‑sparing effect | Moderate | Low |
| Vasodilatory action | Yes (calcium‑channel & nitric‑oxide) | Minimal |
| Preferred use | Hypertension, especially in elderly | Fluid overload, combination therapy |
Practical Considerations for Patients and Clinicians
When starting Indapamide, clinicians usually begin with a low dose (1.5 mg) and monitor blood pressure, electrolytes, and kidney function after one week. Common side effects include mild headache, dizziness, and occasional low potassium. Because the drug is partly excreted unchanged, patients with severe renal impairment (eGFR < 30 mL/min) may need dose adjustments or an alternative.
Drug interactions are relatively few, but combining Indapamide with other potassium‑sparing agents (e.g., spironolactone) can push potassium too high. Likewise, non‑steroidal anti‑inflammatory drugs (NSAIDs) may blunt its diuretic effect.
For pregnant women, the FDA classifies Indapamide as Category B, meaning animal studies have not shown risk but there are limited human data. Most clinicians reserve it for cases where the benefit outweighs potential risks.
Quick Takeaways
- Indapamide blocks the Sodium‑Chloride Symporter in the Distal Convoluted Tubule, curbing sodium and water reabsorption.
- It also relaxes arterial smooth muscle by inhibiting Calcium Channels and raising Nitric Oxide levels.
- The dual action yields steady blood‑pressure reductions with a lower risk of electrolyte imbalance.
- Its long half‑life supports once‑daily dosing, making it convenient for older patients.
- Compared with Hydrochlorothiazide, Indapamide offers better potassium retention and added vasodilation.
Frequently Asked Questions
How quickly does Indapamide start lowering blood pressure?
Blood‑pressure effects can be seen within 24 hours, but the full therapeutic effect usually stabilizes after 2‑3 weeks of consistent dosing.
Does Indapamide cause weight loss?
Any weight loss is modest and comes from fluid reduction, not fat loss. Patients typically lose 1‑2 kg in the first week if they’re fluid‑overloaded.
Can I take Indapamide with my blood‑pressure pill?
Yes, Indapamide is often combined with ACE inhibitors, ARBs, or calcium‑channel blockers for stronger control. The key is to watch electrolytes and kidney function.
What should I avoid while on Indapamide?
Limit high‑salt foods, avoid excessive alcohol, and be cautious with NSAIDs because they can reduce the drug’s diuretic effect.
Is Indapamide safe for people over 65?
It’s actually favored for older adults because the lower dose causes fewer electrolyte shifts and the once‑daily schedule improves adherence.


