Polypharmacy: When Too Many Medications Become a Risk
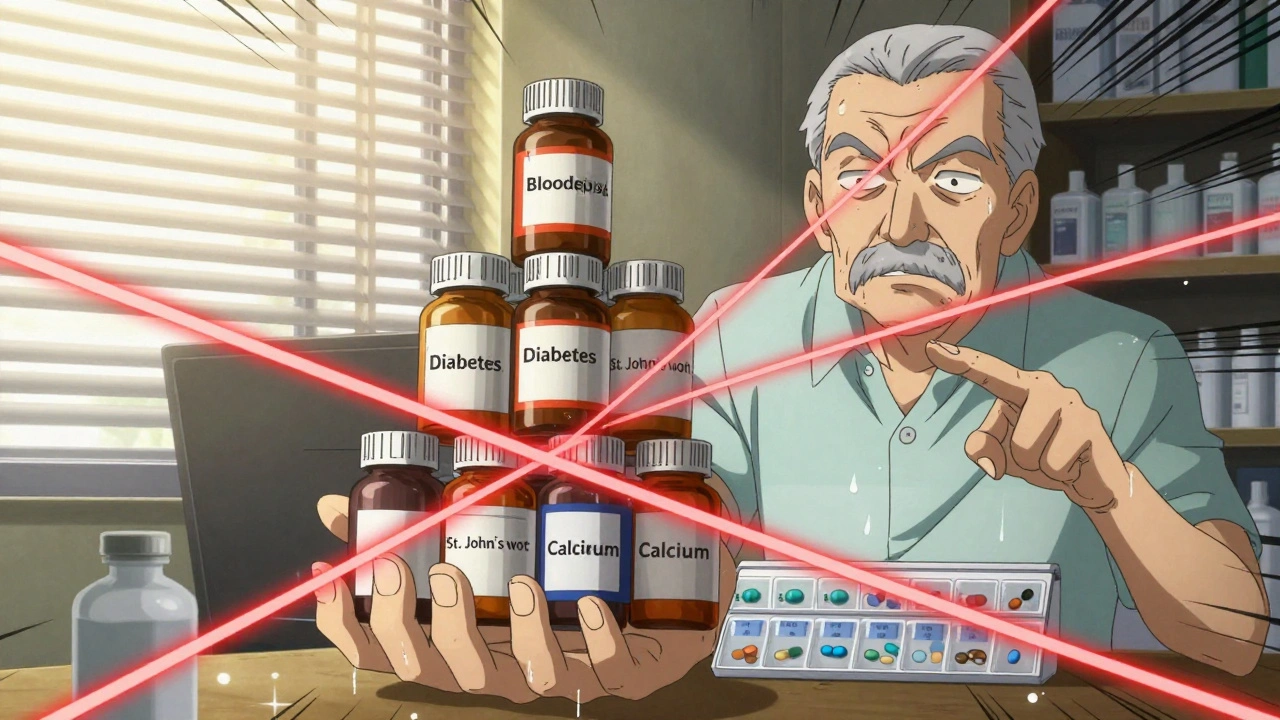
When someone takes polypharmacy, the use of five or more medications at the same time. Also known as multiple medication use, it’s common among older adults managing chronic conditions—but it’s not harmless. Every extra pill adds risk: interactions, side effects, confusion, and even falls. It’s not about how many drugs you’re on—it’s whether each one still serves a real purpose.
Many people don’t realize that medication interactions, when two or more drugs react in harmful ways inside the body. Also known as drug-drug interactions, they can turn a safe treatment into a danger. For example, mixing a blood thinner with an herbal supplement like goldenseal can spike bleeding risk. Or taking multiple drugs that slow your breathing—like painkillers and sleep aids—can stop it altogether. These aren’t rare accidents. They’re predictable, preventable, and happening every day. And the people most at risk? Seniors who see multiple doctors, get prescriptions from different pharmacies, and don’t know what’s in their own medicine cabinet.
deprescribing, the careful process of reducing or stopping medications that are no longer needed or are doing more harm than good. Also known as medication review, it’s not about cutting pills blindly—it’s about smart, step-by-step decisions. Doctors and pharmacists now use tools to map out every drug a patient takes, check for overlaps, and ask: Is this still helping? Could this be causing more problems than it solves? The goal isn’t to stop everything—it’s to stop what’s unnecessary. That’s how you get back control of your health, not your pill organizer.
You’ll find real stories here: how a senior cut six pills down to three and stopped feeling dizzy. How a heart patient avoided a hospital trip by asking about a drug that was masking another problem. How a simple conversation with a pharmacist revealed a dangerous mix of over-the-counter meds and prescriptions. These aren’t theoretical risks—they’re daily realities for millions. And the solutions? They’re simpler than you think. You don’t need a PhD in pharmacology. You just need to know what to ask, what to watch for, and when to push back.
Below, you’ll find clear, no-fluff guides on how to spot trouble before it happens, how to talk to your doctor about cutting back, and how to keep your meds safe and simple. No jargon. No scare tactics. Just what works.