More than 4 in 10 adults over 65 in the U.S. take five or more prescription drugs every day. For many, it’s not a choice-it’s a necessity. Heart disease, diabetes, arthritis, high blood pressure, depression-each condition brings its own pill. But when those pills stack up, so do the risks. polypharmacy isn’t just about taking a lot of meds. It’s about the hidden dangers that come when drugs clash, when side effects create new problems, and when no one stops to ask if you still need them all.
What Makes Polypharmacy Dangerous?
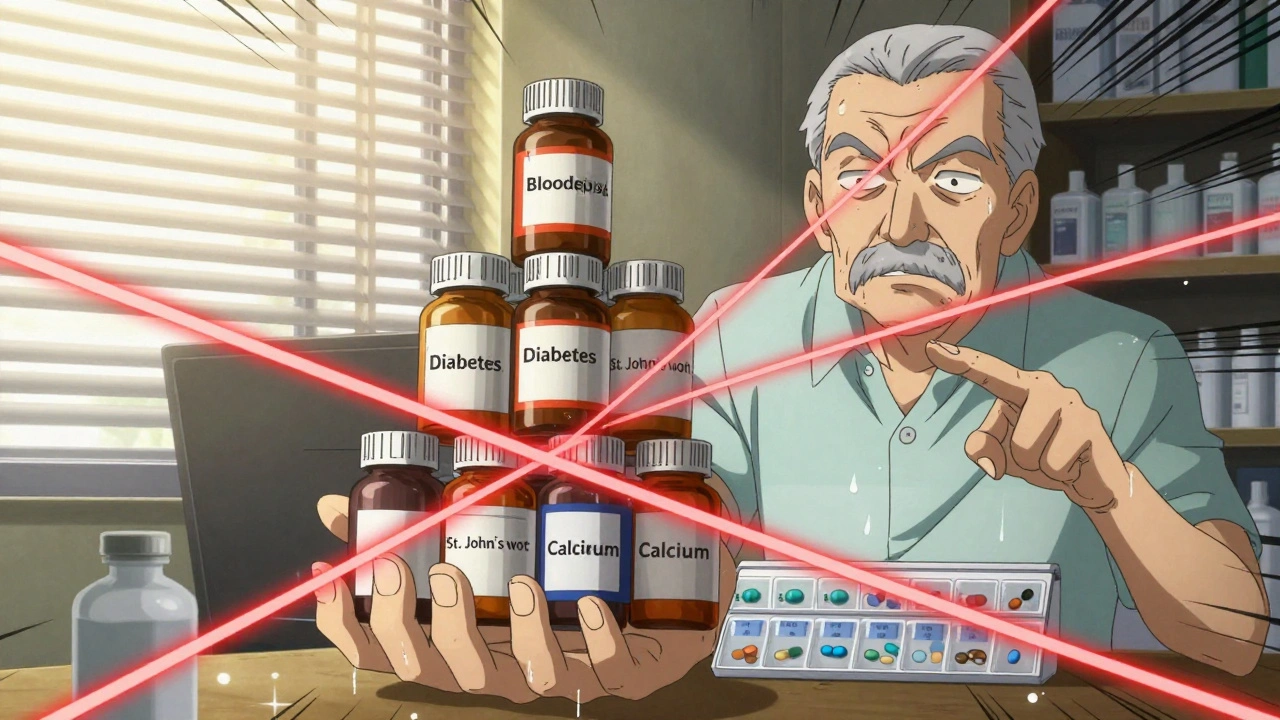
Polypharmacy means taking five or more medications regularly. That number isn’t arbitrary. Studies show that once you hit five, your chance of a harmful drug interaction jumps sharply. It’s not just about two pills reacting badly. It’s about the ripple effect: one drug causes dizziness, so you get a fall-prevention med. That new med lowers your blood pressure too much, so now you need a stimulant. And on it goes-what’s called a prescribing cascade. The real problem? Many of these meds were never meant to be taken together. A 2023 review from the National Center for Biotechnology Information found that nearly 30% of older adults on five or more drugs are taking at least one that doesn’t match their current condition. Some were prescribed years ago and never reviewed. Others were added to treat side effects of another drug, creating a cycle no one noticed. And it’s not just prescriptions. Over-the-counter painkillers, herbal supplements, vitamins, sleep aids-many people don’t think of these as "medications." But they can be just as risky. St. John’s Wort can make your blood thinner useless. Calcium supplements can block your thyroid med. Even grapefruit juice can turn a common cholesterol drug into a dangerous overdose.How to Know If You’re in Risky Territory
Ask yourself these questions:- Do you take more than five medications daily-including vitamins or OTC drugs?
- Have you ever been told to stop a drug but never got clear instructions?
- Do you ever feel more tired, dizzy, confused, or nauseous after starting a new pill?
- Do you use more than one pharmacy or get prescriptions from different doctors?
- Have you ever skipped a dose because the schedule was too confusing?
Five Steps to Manage Your Meds Safely
The World Health Organization laid out a clear, proven approach. You don’t need to be a doctor to use it. Here’s how to apply it to your life.- Make a complete list-every pill, patch, capsule, and drop. Include brand names, generic names, dosages, times of day, and why you’re taking each one. Don’t forget supplements. Write it down. Don’t rely on memory. Keep a copy in your wallet and another on your phone.
- Bring your list to every appointment-even if it’s just for a cold. Show it to your doctor, pharmacist, nurse, or whoever you see. If you’re seeing multiple providers, make sure they all have the same list. A 2023 study showed that patients who brought their full med list to visits had 40% fewer dangerous interactions.
- Use one pharmacy-always. That way, the pharmacist can flag dangerous combinations before you even leave the store. Pharmacists are trained to spot interactions. But they can’t help if you’re picking up meds from five different places.
- Ask: "Is this still needed?"-at every visit. Don’t wait for your doctor to bring it up. Say: "I’m on a lot of meds. Is there one I can stop?" Many drugs lose their benefit over time. Blood pressure meds for mild hypertension, sleep aids after a few months, acid reducers for occasional heartburn-these are common candidates for deprescribing.
- Never stop or change a med on your own. Some drugs, like antidepressants or heart meds, can cause serious withdrawal or rebound effects if stopped suddenly. Always talk to your provider first.
Deprescribing: Stopping Meds Can Be Just as Important as Starting Them
Deprescribing isn’t about cutting corners. It’s about smart medicine. It means stopping drugs that no longer help-or that now hurt more than they help. The American Academy of Family Physicians says deprescribing should be a routine part of care, not an afterthought. But it’s not just about reducing numbers. It’s about matching meds to your current health goals. If you’re 85 with advanced heart failure, do you still need a statin for cholesterol you’ve had for 30 years? Maybe not. If your goal is comfort and quality of life, not extending life by a few months, some meds become unnecessary. A 2024 study in the Journal of the American Geriatrics Society found that patients who had a structured deprescribing plan reported fewer side effects, less confusion, and better sleep-all without worsening their original conditions. The key? Work with your provider. Don’t just stop. Taper. Monitor. Reassess. Some meds can be cut quickly. Others need weeks or months to come off safely. Your pharmacist can help you create a safe plan.How to Talk to Your Doctor About Your Meds
It’s easy to feel like you’re bothering your doctor. You’re not. You’re doing your job. Here’s what to say:- "I’ve been taking this for years. Is it still helping?"
- "I’ve noticed I feel more tired since I started this new pill. Could it be related?"
- "I’m worried about taking so many. Can we look at what’s essential?"
- "Can we try stopping this one for a few weeks and see how I feel?"
Build a Routine That Works
Taking meds consistently is half the battle. But if you’re juggling 10 pills at different times of day, it’s easy to miss one-or double up. Try this: link each pill to a daily habit.- Take your blood pressure pill with your morning coffee.
- Take your diabetes med right after brushing your teeth.
- Put your nighttime pill next to your toothbrush.
When to Call for Help
You don’t need to wait for a bad reaction. Watch for these signs:- New confusion or memory lapses
- Unexplained falls or dizziness
- Sudden fatigue or weakness
- Loss of appetite or weight loss
- Upset stomach, nausea, or diarrhea that started after a new med
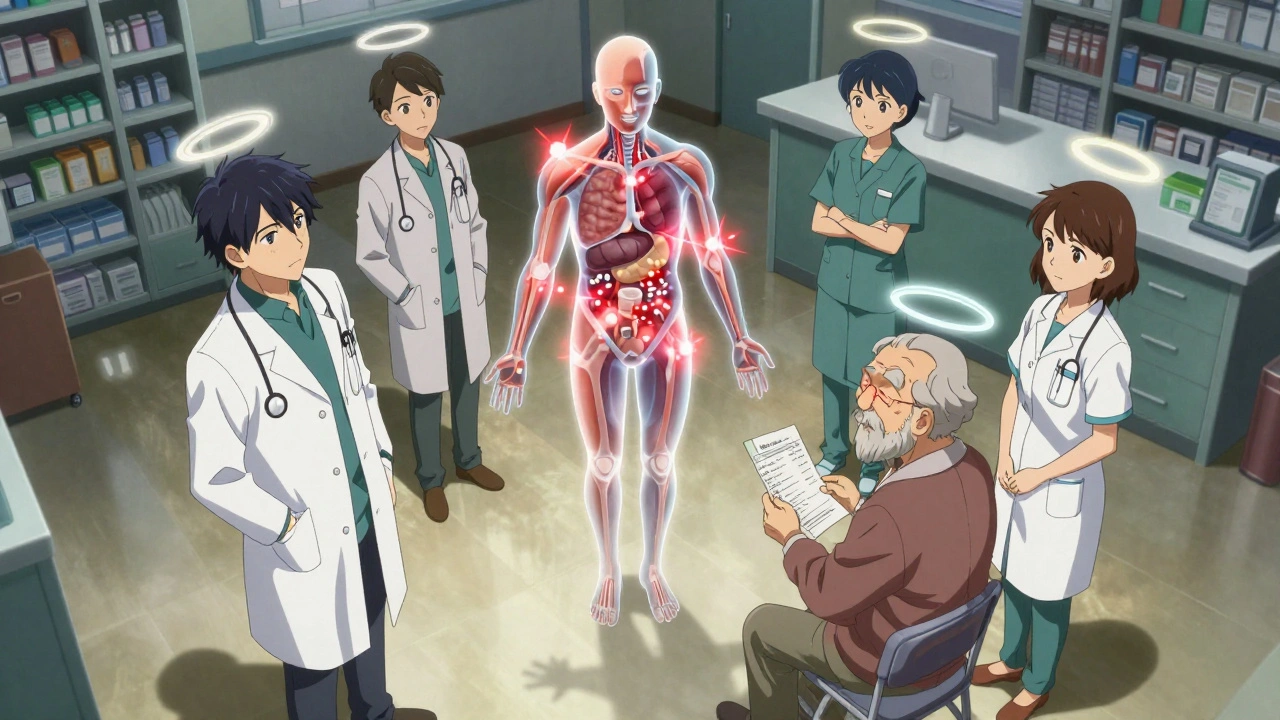
Teamwork Makes It Work
No one person should manage your meds alone. Your doctor prescribes. Your pharmacist checks for clashes. Your nurse helps with reminders. Your caregiver watches for changes. You’re the most important part-you know how you feel. Ask your doctor if they have a care team that includes a pharmacist. Many clinics now have clinical pharmacists on staff whose only job is to review complex med regimens. Ask if you can get one. And if you’re switching hospitals or moving to a rehab center, make sure your full med list goes with you. Medication errors are most common during transitions. A 2023 study found that 70% of these errors happen because the new team didn’t have the full picture.You’re Not Alone
Managing multiple meds is hard. It’s confusing. It’s overwhelming. But you don’t have to do it alone. Millions of people are in the same boat. The goal isn’t to take fewer pills for the sake of it. The goal is to take only what helps you live better, safer, and with fewer side effects. Start small. Make your list. Bring it to your next visit. Ask one question. That’s enough to start changing things.What is polypharmacy?
Polypharmacy means taking five or more medications at the same time regularly. It’s common in older adults and people with multiple chronic conditions. While sometimes necessary, it increases the risk of harmful drug interactions, side effects, and medication errors.
Are over-the-counter drugs and supplements part of polypharmacy?
Yes. Over-the-counter pain relievers, sleep aids, antacids, and herbal supplements like St. John’s Wort or garlic pills can interact with prescription drugs. Many people don’t realize these count as medications, but they’re often the hidden cause of dangerous reactions. Always include them on your medication list.
Can I stop taking a medication if I think it’s not helping?
No. Some medications, like blood pressure drugs, antidepressants, or seizure meds, can cause serious withdrawal symptoms or rebound effects if stopped suddenly. Always talk to your doctor or pharmacist first. They can help you safely taper off if it’s the right choice.
What is deprescribing?
Deprescribing is the planned, supervised process of stopping medications that are no longer needed or that may be doing more harm than good. It’s not about cutting pills for the sake of fewer numbers-it’s about matching your meds to your current health goals, especially as you age or your condition changes.
How often should I review my medications?
At least once a year, or anytime you see a new doctor, start a new medication, or notice new side effects. Many experts recommend reviewing your meds at every health maintenance visit. Keep your list updated and bring it to every appointment.
Can a pharmacist help me manage my meds?
Yes. Pharmacists are trained to spot dangerous drug interactions, check for duplicate prescriptions, and identify medications that may no longer be necessary. Many pharmacies now offer free med reviews. Ask if your pharmacy has a clinical pharmacist on staff who can help you with complex regimens.