Goldenseal Medication Interaction Checker
Goldenseal Medication Interaction Checker
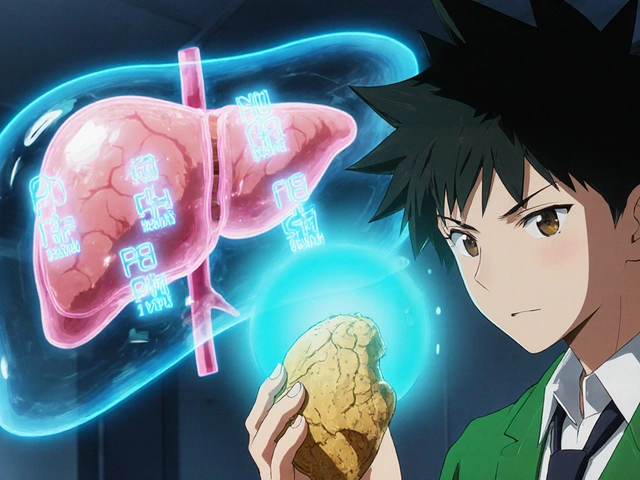
Goldenseal can inhibit key liver enzymes that metabolize many medications. This tool helps you check if your current medications are at risk when using goldenseal.
Based on research, goldenseal inhibits five major CYP enzymes (CYP3A4, CYP2D6, CYP2C9, CYP1A2, and CYP2E1), which could lead to increased medication levels and potential side effects.
Select Your Medications
Quick Takeaways
- Goldenseal inhibits five major CYP enzymes, especially CYP2E1 and CYP3A4.
- Inhibition can raise blood levels of drugs such as warfarin, statins, metoprolol, and digoxin.
- Even low‑dose supplements show variable berberine content, making effects unpredictable.
- Most experts advise avoiding goldenseal if you’re on any prescription that relies on CYP metabolism.
- A 2‑week wash‑out after stopping goldenseal is usually needed before starting or adjusting sensitive meds.
People turn to goldenseal for a quick immune boost or to soothe sinus congestion, but the herb carries a hidden danger: it can slam the brakes on liver enzymes that clear most prescription drugs. When those enzymes are blocked, medication levels can spike, side‑effects can worsen, and therapeutic outcomes can derail. This article breaks down exactly how goldenseal interacts with liver enzymes, which drugs are most at risk, and what clinicians and patients should do to stay safe.
What is Goldenseal?
Goldenseal is a perennial herb (Hydrastis canadensis) native to eastern North America. Historically, Native American healers used the root and rhizome for infections, inflammation, and digestive upset. Modern manufacturers market it as a dietary supplement for immune support and sinus relief, even though the FDA has not approved any therapeutic claim (2022). Commercial products typically supply 0.5‑1 g of dried root three times daily, or liquid extracts ranging from 0.3 ml to 4 ml per dose.
How Goldenseal Affects Liver Enzymes
The liver’s cytochrome P450 (CYP) system is the workhorse that metabolises roughly three‑quarters of all prescription medicines. Goldenseal’s two major alkaloids-berberine and hydrastine-act like a broad‑spectrum inhibitor, slowing down several CYP isoforms at once. Inhibiting these enzymes means drugs stay in the bloodstream longer, often at higher concentrations than intended.
Key CYP Isoforms Inhibited by Goldenseal
Research consistently points to five CYP enzymes most affected:
- CYP3A4 (handles ~50 % of all drugs, including statins, immunosuppressants, benzodiazepines) - average inhibition ~48 %.
- CYP2D6 (metabolises ~30 % of meds such as codeine, fluoxetine, metoprolol) - inhibition ~55 %.
- CYP2C9 (important for warfarin, certain NSAIDs) - inhibition ~45 %.
- CYP1A2 (metabolises caffeine, clozapine, theophylline) - inhibition ~63 %.
- CYP2E1 (handles acetaminophen, low‑dose ethanol) - inhibition ~78 % (the strongest effect reported).
Because the herb hits multiple pathways at once, the overall interaction risk is higher than most single‑enzyme inhibitors.
Clinical Impact on Common Medications
When a drug depends on one of the inhibited CYPs, goldenseal can push blood levels up by 40‑60 % or more. Here are the most frequently cited scenarios:
- Warfarin: INR may rise 1.5‑2.0 points, increasing bleeding risk.
- Statins (simvastatin, atorvastatin): higher muscle‑toxic concentrations, potential rhabdomyolysis.
- Metoprolol and other beta‑blockers: exaggerated heart‑rate slowing, dizziness.
- Codeine and tramadol: increased conversion to active metabolites, raising sedation and respiratory depression.
- Digoxin: berberine also blocks P‑glycoprotein, raising digoxin levels up to 30‑40 %.
- Acetaminophen: CYP2E1 inhibition reduces toxic metabolite formation, but the FDA warning emphasizes that altered metabolism can still cause unpredictable liver stress.
A 2018 trial showed that patients on CYP2D6 substrates experienced a 45 % rise in plasma drug concentration after just a week of goldenseal (500 mg/day). The effect lingered for up to two weeks after stopping the herb.
How Goldenseal Stacks Up Against Other Herbs
Herbal supplements vary widely in how they interact with CYP enzymes. The table below contrasts goldenseal with three well‑known herbs.
| Herb | Main Active(s) | Enzyme(s) Inhibited | Enzyme(s) Induced | Relative Interaction Risk |
|---|---|---|---|---|
| Goldenseal | Berberine, Hydrastine | CYP3A4, CYP2D6, CYP2C9, CYP1A2, CYP2E1 | None | High (3rd‑highest among 15 studied) |
| Milk Thistle | Silymarin | CYP2C9 (moderate) | None | Low‑Medium |
| St. John’s Wort | Hypericin, Hyperforin | None | CYP3A4 (strong inducer) | Very High (can reduce drug levels 70‑80 %) |
| Grapefruit Juice | Furanocoumarins | CYP3A4 (strong inhibitor) | None | High (but limited to CYP3A4) |
The key takeaway: goldenseal’s multi‑enzyme blockade makes it riskier than herbs that affect only one pathway.
Practical Guidance for Patients and Providers
Given the evidence, most clinicians apply a “5‑CYP Rule”: if a patient is taking any medication metabolised by CYP3A4, CYP2D6, CYP2C9, CYP1A2, or CYP2E1, goldenseal should be avoided.
- Screening: Ask every patient about supplement use, especially before prescribing new drugs.
- Wash‑out: Discontinue goldenseal at least 14 days before starting a CYP‑sensitive medication.
- Monitoring: If goldenseal was taken inadvertently, check drug levels (e.g., INR for warfarin, serum digoxin) and adjust doses as needed.
- Patient education: Explain that “natural” does not equal “safe” and that supplement labels often hide the exact berberine concentration.
Pharmacists can use the American Society of Health‑System Pharmacists’ online CYP interaction checker, which lists 147 medications with documented or theoretical goldenseal interactions (updated Q3 2023).
Monitoring and Managing Interactions
If a patient insists on using goldenseal despite the risks, adopt a mitigation strategy:
- Document the exact product, dose, and form (capsule, tincture, extract).
- Order baseline labs relevant to the medication (e.g., INR, liver enzymes, fasting glucose).
- Schedule follow‑up within 1‑2 weeks to reassess lab values and symptoms.
- If labs shift beyond therapeutic windows, advise immediate discontinuation and consider alternative therapies.
Remember that the inhibition effect can linger for up to two weeks after the last dose, so timing of lab repeats matters.
Regulatory Landscape and Ongoing Research
The FDA classifies goldenseal as a dietary supplement under DSHEA, meaning it cannot make disease‑treatment claims. However, warning letters in 2021 targeted manufacturers that overstated benefits. The European Medicines Agency has outright rejected goldenseal for medicinal use.
In September 2023, the National Institutes of Health launched a $2.3 million clinical trial (NCT05578231) to evaluate goldenseal’s interaction profile with ten common drugs in healthy volunteers. Results are expected by Q3 2025 and may reshape guidance.
Adverse‑event reporting to the FDA rose 37 % from 2018‑2022, highlighting growing awareness but also persistent use. Market analysts estimate U.S. goldenseal sales at $18.7 million in 2022, showing demand outpaces safety messaging.
Bottom line: goldenseal’s broad CYP inhibition makes it a high‑risk supplement for anyone on prescription medication. Until robust human trials clarify safe dosing, the safest path is to avoid it-or at the very least, to coordinate its use under close medical supervision.
Frequently Asked Questions
Can I take goldenseal with blood pressure medication?
Most blood‑pressure drugs are metabolised by CYP2D6 or CYP3A4, so goldenseal can raise their levels and cause dizziness or dangerous drops in blood pressure. The consensus is to avoid the combination.
How long does the enzyme inhibition last after stopping goldenseal?
Studies in rats and humans suggest inhibition can persist 7‑14 days. A two‑week wash‑out is the most conservative recommendation.
Is berberine the only risky component?
Berberine is the main culprit, but hydrastine also contributes to CYP inhibition, and both vary wildly between brands. That variability makes dose‑response predictions unreliable.
Are there any safe situations to use goldenseal?
Short‑term use (3‑5 days) for acute sinus infections, **without** any concurrent prescription meds, is the only scenario where risk is minimal. Even then, monitor for side‑effects.
What alternatives can I consider for immune support?
Probiotics, vitamin C, and zinc have solid safety profiles and no known CYP interactions. Discuss any supplement with your pharmacist before adding it to your regimen.