When two or more drugs are combined into a single pill or formulation, getting the dose right isn’t just about matching numbers-it’s about making sure the body responds the same way every time. This is where therapeutic equivalence comes in. It’s not enough for two combination products to have the same active ingredients. They must deliver those ingredients in a way that produces identical clinical results. And when doses vary-even slightly-things get complicated fast.
What Therapeutic Equivalence Really Means
Therapeutic equivalence isn’t a marketing term. It’s a scientific and regulatory standard defined by the FDA. Two drug products are therapeutically equivalent if they contain the same active ingredients, in the same strength, dosage form, and route of administration, and they work the same way in the body. The FDA tracks these in the Orange Book, where over 14,000 products have been rated. About 95% of them carry an ‘A’ rating, meaning they can be substituted without concern. But here’s the catch: this only applies when the doses are identical. If you switch from a 5mg/10mg combination to a 10mg/20mg version, even if both are labeled as the same drug, you’re no longer dealing with therapeutic equivalence-you’re dealing with a different treatment entirely.Why Dose Differences Break Equivalence
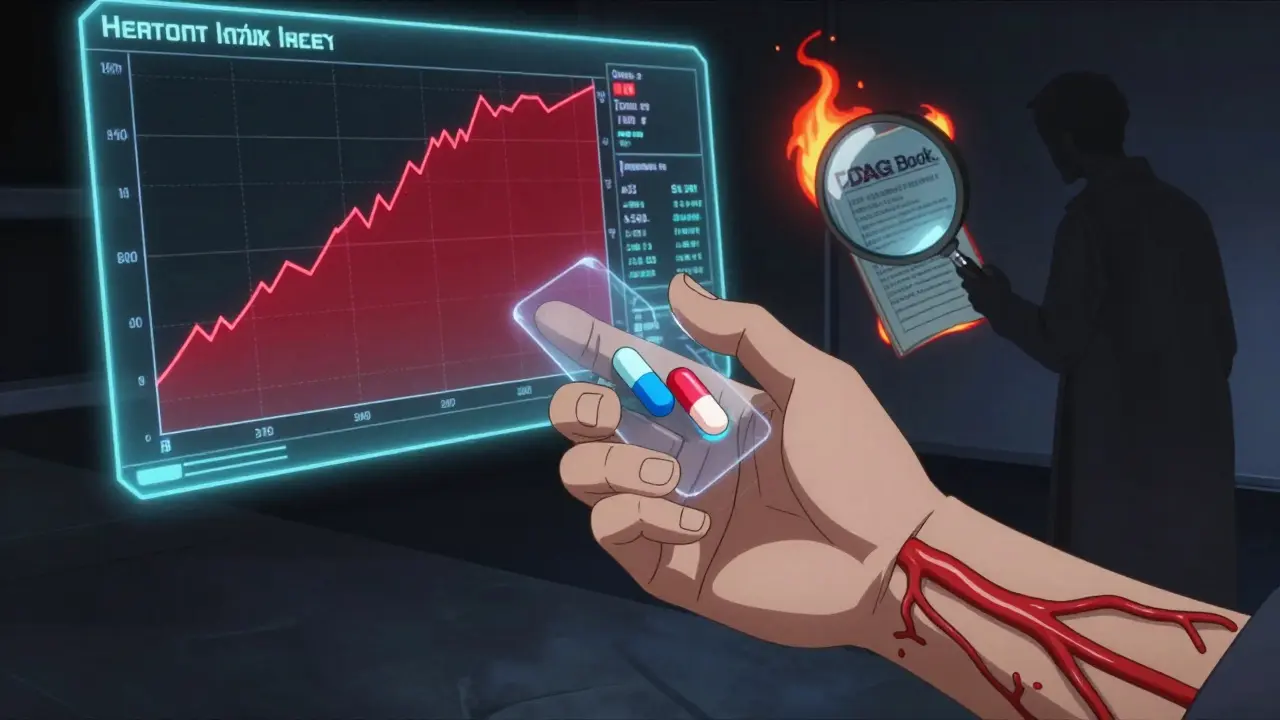
Combination products like amlodipine/benazepril (for high blood pressure) or ezetimibe/simvastatin (for cholesterol) are designed to work together. The doses are chosen based on clinical trials that tested specific ratios. Swap one component’s dose, and you change the whole balance. Take the case of tramadol and acetaminophen. One study showed that when combined, the pain relief wasn’t just the sum of each drug’s effect-it was stronger. That’s called synergy. But if you substitute a version with a lower dose of tramadol, even if it’s labeled as “therapeutically equivalent,” you might lose that synergy. The patient gets less relief, and the risk of rebound pain goes up. This is especially dangerous with narrow therapeutic index (NTI) drugs. These are medications where the difference between a helpful dose and a toxic one is tiny. Think warfarin, levothyroxine, or phenytoin. When these are part of a combination, even small differences in absorption-caused by different inactive ingredients-can lead to serious side effects. A 2018 study found that 12% of patients switching between generic levothyroxine products had abnormal thyroid levels, even though the FDA approved both as equivalent.How the FDA Rates Combination Products
The FDA doesn’t just look at the active ingredients. It checks bioequivalence: how much of the drug enters the bloodstream and how fast. For most drugs, a product is considered equivalent if its absorption falls within 80-125% of the brand. But for NTI drugs in combinations, that range tightens to 90-111%. That’s because small changes matter more. Combination products get a TE code in the Orange Book. The first letter tells you the story:- A = Therapeutically equivalent. Safe to substitute.
- B = Not equivalent. Bioequivalence hasn’t been proven, or there are unresolved issues.
Real-World Mistakes Happen
Pharmacists aren’t the only ones confused. A nurse practitioner on Allnurses.com described a patient switched from brand-name Vytorin (ezetimibe/simvastatin 10/20mg) to a generic. LDL cholesterol rose by 15%. The generic met FDA standards-but the patient’s body responded differently. Why? The inactive ingredients altered how the simvastatin was released. Another case from Reddit: a pharmacist with 12 years of experience reported three dosing errors in six months just from switching between different strengths of amlodipine/benazepril. One patient got 10mg/40mg instead of 5mg/20mg. The result? Dizziness, low blood pressure, and a trip to the ER. The FDA’s own adverse event database recorded 247 incidents in 2022 tied to dose conversion errors in combination products. Nearly 40% involved heart medications. Another 30% involved antidepressants or antipsychotics-drugs where even small changes in blood levels can trigger agitation, seizures, or suicidal thoughts.How to Manage Dose Changes Safely
There’s no magic fix, but there are proven steps to reduce risk:- Check the Orange Book. Never assume two products are interchangeable. Look up the TE code. If it’s ‘A,’ you’re good-if the doses match exactly.
- Never switch doses without a new prescription. If a patient needs a different strength, the prescriber must write it explicitly. Don’t rely on “they’re the same.”
- Use barcode scanning. Systems that require scanning before dispensing reduce substitution errors by up to 65%, according to the University of California Health System.
- Monitor high-risk patients for 72 hours. After switching any combination product with NTI components, check labs, blood pressure, or symptoms. Don’t wait for the patient to come back.
- Keep standardized conversion tables. For common combinations like metoprolol/valsartan or oxycodone/acetaminophen, have a printed or digital reference handy. Don’t calculate on the fly.
The Future: Personalized Equivalence?
The FDA is already working on new tools. In 2023, they released a draft guidance for complex combination products-those where dose-response isn’t linear. They’re also testing machine learning models that predict which generic substitutions might fail based on formulation differences. Early results show 89% accuracy. Long-term, the goal is to move beyond one-size-fits-all equivalence. By 2030, the NIH predicts that 30% of therapeutic equivalence decisions will include pharmacogenomic data. That means your genes-how fast you metabolize a drug-will help determine whether a generic is truly equivalent for you. Until then, the rule is simple: if the dose changes, it’s not the same drug. And if you’re managing combinations, treat every substitution like a clinical decision-not just a billing one.Frequently Asked Questions
Can I substitute a generic combination product if the brand and generic have the same TE code?
Yes-but only if the doses are identical. A TE code of ‘A’ means the active ingredients, strengths, dosage form, and route are the same. If one product is 5mg/10mg and the other is 10mg/20mg, they’re not interchangeable, even if both are rated ‘A.’ Always check the strength on the label.
Why do some generic combination products cause side effects when the brand doesn’t?
Inactive ingredients-like fillers, coatings, or disintegrants-can change how quickly the drug is absorbed. For NTI drugs like warfarin or levothyroxine, even small differences in absorption can push levels into the toxic range. The FDA approves generics based on average bioequivalence, not individual response. Some patients are more sensitive to these formulation differences.
Are combination products with different manufacturers always interchangeable?
Not always. Two products can have the same TE code but different inactive ingredients. For example, rivaroxaban generics vary in disintegrants. In a combination with another drug, this can affect absorption timing. Always verify the manufacturer and check for any patient-specific history of reactions to certain fillers.
How do I know if a combination product has a narrow therapeutic index?
Common NTI drugs include warfarin, levothyroxine, phenytoin, lithium, carbamazepine, and cyclosporine. If any of these are part of a combination, treat it with extra caution. Check the FDA’s list of NTI drugs or consult a clinical pharmacist. Never assume a combination is safe to swap without verifying the components.
What should I do if a patient has a bad reaction after switching to a generic combination?
Immediately return the patient to the original product. Document the reaction and report it to the FDA’s MedWatch program. Notify the prescriber and pharmacy. If the reaction was serious, consider filing a report with the Institute for Safe Medication Practices. Many errors go unreported-your report could prevent another incident.