Managing diabetes isn’t about cutting out carbs entirely-it’s about knowing exactly how much you’re eating and how it affects your blood sugar. That’s where carbohydrate counting comes in. It’s not a diet. It’s not a restriction. It’s a tool. And if you’re on insulin or trying to get your blood sugar under control, it’s one of the most powerful tools you can learn.
Why Carbohydrate Counting Matters
Carbs are the main nutrient that raises your blood sugar. Whether it’s bread, rice, fruit, or even milk, every gram of carbohydrate turns into glucose after digestion. If you’re taking insulin, your body needs a matching amount to handle that glucose. Too many carbs without enough insulin? Blood sugar spikes. Too few carbs with too much insulin? Dangerously low blood sugar. Carb counting gives you control. Instead of guessing or following rigid meal plans, you learn to match your food to your insulin. The American Diabetes Association (ADA) recommends it as a proven method for people with type 1 diabetes and many with type 2 who use insulin. Studies show people who count carbs regularly see HbA1c drops of 0.5% to 1.0%-enough to reduce long-term complications like nerve damage, kidney issues, and vision loss.What Counts as One Carb Serving?
Carbs are measured in grams. One standard serving equals about 15 grams of total carbohydrates. That’s the building block of carb counting. Here’s what 15 grams of carbs looks like in real life:- 1 small apple (about the size of a tennis ball)
- 1 slice of whole wheat bread
- 1/2 cup of cooked pasta or rice
- 1/2 cup of beans or lentils
- 1 cup of milk or plain yogurt
- 1/3 cup of cooked oatmeal
- 1/2 cup of canned fruit in juice (not syrup)
Reading Nutrition Labels Like a Pro
The key is the “Total Carbohydrate” line on the nutrition facts label. Ignore sugar, fiber, or “net carbs” for now. Just look at the total. Let’s say a cereal box says: Total Carbohydrate: 30g per serving. That’s two carb servings. If you eat two servings, that’s 60 grams-four carb servings. But here’s the trick: fiber and sugar alcohols don’t always count the same way.- If a food has more than 5 grams of fiber per serving, subtract the full amount of fiber from total carbs.
- If it contains sugar alcohols (like erythritol or maltitol), subtract half of the sugar alcohol grams.
Your Carb Target: No One-Size-Fits-All
There’s no magic number. Your daily carb goal depends on your weight, activity level, insulin sensitivity, and blood sugar goals. Most adults with type 1 diabetes eat between 150 and 250 grams of carbs per day. That’s 10 to 16 carb servings. People with type 2 diabetes may aim lower-100 to 150 grams-especially if they’re trying to lose weight. But here’s the truth: your doctor or certified diabetes educator will help you find your personal number. One person might need 45% of calories from carbs. Another might do better with 55%. It’s not about what’s “healthy” for everyone-it’s what works for you.Matching Carbs to Insulin: The Ratio That Changes Everything
If you take insulin, you need a carb-to-insulin ratio. This tells you how many units of insulin to take per gram of carbs. A common starting point is 1:10-meaning 1 unit of insulin for every 10 grams of carbs. But your ratio might be 1:8, 1:12, or even 1:15. Your ratio isn’t set in stone. It changes depending on the time of day. Many people need more insulin for breakfast (called “dawn phenomenon”) and less at dinner. Example: You’re eating a sandwich with 45 grams of carbs. Your ratio is 1:10. So you take 4.5 units of insulin. This is where carb counting becomes powerful. You’re not eating a fixed meal-you’re adjusting based on what’s on your plate.
Tools You Actually Need to Start
You don’t need fancy gear. But you do need a few basics to get accurate:- A food scale (for meats, cheese, and dry goods)
- Measuring cups and spoons (for rice, pasta, cereal)
- A calculator or phone app
- A food diary or app like MyFitnessPal or Carb Manager
Where People Go Wrong (And How to Fix It)
Most beginners make the same mistakes:- Forgetting carbs in sauces, dressings, and condiments. Ketchup has 4g of carbs per tablespoon. Mayo? Zero. But salad dressing? Often 5-10g per serving.
- Not counting starchy vegetables. Sweet potatoes, corn, peas, and carrots all count as carbs. They’re healthy-but they still raise blood sugar.
- Assuming “sugar-free” means “carb-free.” Sugar-free cookies often have 20g+ of carbs from flour and fillers.
- Ignoring restaurant meals. A “small” pasta dish at a restaurant can have 80-100g of carbs-not the 45g you’d expect.
Carb Counting vs. Other Methods
You might hear about the “plate method” or “glycemic index.” Here’s how carb counting stacks up:- Plate Method: Fill half your plate with non-starchy veggies, a quarter with protein, a quarter with carbs. Simple-but no numbers. You won’t know if you’re eating 30g or 80g of carbs.
- Glycemic Index (GI): Focuses on how fast carbs raise blood sugar. Low-GI foods are better, but it doesn’t tell you how much you’re eating. You could eat a low-GI food in huge amounts and still spike.
- Carb Counting: Tells you exactly how much you’re eating. You can eat high-GI foods (like white rice) if you adjust your insulin. You can eat low-GI foods (like lentils) and still overdo it.
What About Continuous Glucose Monitors (CGMs)?
If you use a CGM, carb counting gets even better. You’ll see real-time spikes after meals. Did your blood sugar jump 80 points after eating a banana? That tells you your carb count was off-or your insulin timing was late. CGMs turn carb counting from theory into feedback. You can test: “What happens if I eat 30g of carbs with 3 units of insulin?” Then check your graph 2 hours later. Adjust. Try again. It’s like having a coach in your pocket.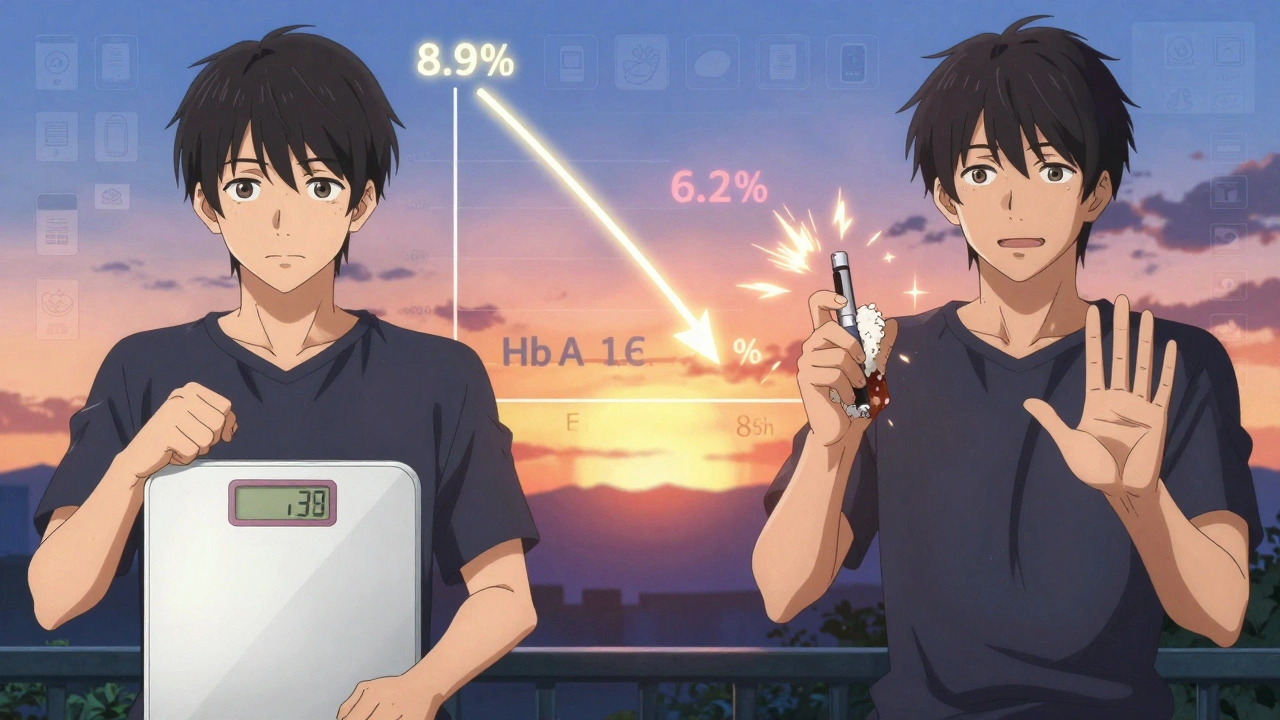
How Long Until You Get Good at This?
It takes time. Most people take 4 to 8 weeks to feel confident. In the first month, you’ll spend 30 to 60 minutes per meal measuring, logging, calculating. That’s exhausting. But here’s the good news: after 30 days, you’ll cut that time in half. After two months, you’ll estimate accurately 85% of the time. Don’t quit because it feels hard at first. Every expert started where you are now.Real People, Real Results
One user on Reddit tracked their carb intake for 3 months. Their post-meal spikes dropped from over 250 mg/dL to 160-180 mg/dL. Another person reduced their HbA1c from 8.9% to 6.2% in 18 months using carb counting and adjusted insulin. It’s not magic. It’s math. And it works.When You Should Skip Carb Counting
Not everyone needs it. If you manage type 2 diabetes with diet and oral meds (like metformin), you might do fine with portion control or the plate method. Carb counting adds complexity without clear benefit if you’re not using insulin. But if you take rapid-acting insulin at meals-whether by injection or pump-carb counting isn’t optional. It’s essential.Where to Get Help
You don’t have to learn this alone. Ask your doctor for a referral to a Certified Diabetes Care and Education Specialist (CDCES). These are registered dietitians or nurses trained specifically in carb counting and insulin dosing. Most hospitals and clinics offer diabetes education classes-often covered by insurance. These classes include hands-on practice with food labels, measuring tools, and insulin calculations. Also, use free tools:- USDA FoodData Central (search any food, get exact carb count)
- MyFitnessPal or Carb Manager (scan barcodes, log meals)
- Diabetes.org (free carb counting worksheets)
Final Thought: It’s About Freedom, Not Restriction
Carb counting doesn’t mean giving up pizza, pasta, or ice cream. It means you can enjoy them-without crashing your blood sugar. You can have a birthday cake if you count the carbs and take the right insulin. You can eat out with friends without fear. This isn’t about being perfect. It’s about being informed. Every gram you count is a step toward better control, fewer spikes, and more confidence. Start small. Measure one meal today. Just one. Write it down. Check your blood sugar two hours later. See what happened. That’s how it begins.Is carb counting only for people with type 1 diabetes?
No. While carb counting is essential for people with type 1 diabetes and those on insulin, it’s also helpful for many with type 2 diabetes-especially if they’re using insulin or want tighter blood sugar control. People managing type 2 with oral meds alone may not need it, but tracking carbs can still improve results.
Do I need to count fiber and sugar alcohols?
Yes, but only in specific cases. If a food has more than 5 grams of fiber per serving, subtract the full amount from total carbs. For sugar alcohols, subtract half. These don’t raise blood sugar like regular carbs, so they shouldn’t be fully counted.
Can I use an app instead of measuring everything?
Apps like MyFitnessPal and Carb Manager are great tools, but they’re only as good as the data you enter. In the beginning, measure your food with a scale and measuring cups to train your eye. After a few weeks, you can rely more on apps-but always double-check labels and restaurant info.
What if I eat out and don’t know the carb count?
Most major restaurant chains list nutrition info online. Search “[restaurant name] nutrition facts.” If you’re at a small place, estimate conservatively. A plate of pasta? Assume 70-80g. A burrito? 60-90g. Better to overestimate than risk a spike. You can always adjust insulin later if your CGM shows you’re low.
How do I know my carb-to-insulin ratio?
Your doctor or diabetes educator will help you calculate it. Start with a common ratio like 1:10, then test after meals. If your blood sugar is still high 2 hours later, you may need more insulin per gram. If it drops too low, you may need less. Adjust slowly and track results over days.
Can I stop carb counting once I get better?
You can reduce how often you measure, but don’t stop tracking entirely. Blood sugar responses change over time due to weight, activity, stress, or medications. Even experienced users check labels and adjust ratios. Carb counting becomes second nature-it’s not a temporary fix, it’s a lifelong skill.


