When the liver gets damaged over time-whether from alcohol, hepatitis, or fatty liver disease-it doesn’t heal the way other organs do. Instead of repairing itself, it builds scar tissue. This scar tissue doesn’t work. It blocks blood flow. And over years, this process turns a healthy liver into something stiff, lumpy, and barely functional. That’s cirrhosis. It’s not just a diagnosis. It’s a tipping point. Once you hit this stage, the body starts falling apart in ways most people don’t expect.
What Cirrhosis Really Does to Your Body
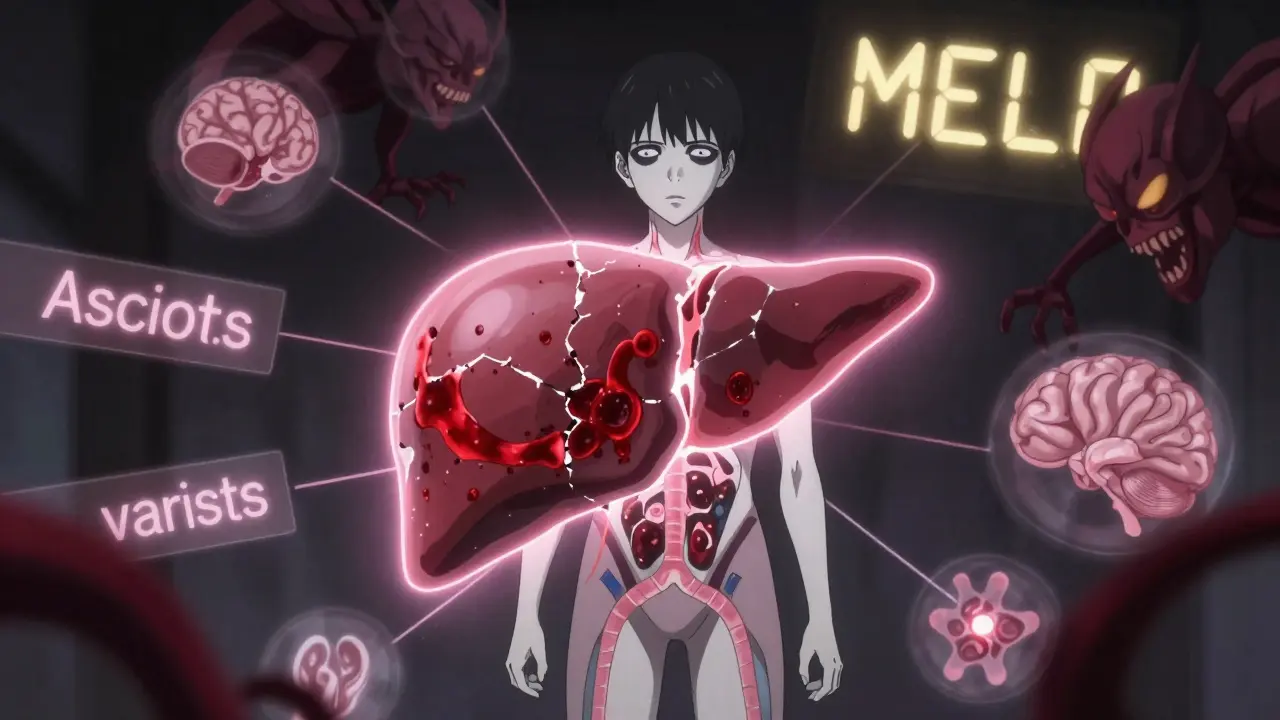
Cirrhosis isn’t one disease. It’s the final result of years of damage. The liver tries to regenerate, but the scar tissue piles up like broken concrete. Blood can’t flow through easily. Pressure builds. And that’s when the real problems start. The first sign for many people is fatigue. Not just tiredness-deep, bone-deep exhaustion that doesn’t go away with sleep. About 72% of people with early cirrhosis report this. Then come the subtle clues: bruising easily, swelling in the legs, unexplained weight loss. These aren’t random. They’re signals your liver is struggling. As things worsen, the body starts breaking down in specific, dangerous ways. Fluid builds up in the belly-ascites. The liver can’t make enough protein to hold fluid in the bloodstream, so it leaks into the abdomen. About half of all cirrhosis patients develop this within ten years. It’s not just uncomfortable. It can get infected. Spontaneous bacterial peritonitis (SBP) kills 20-40% of those who get it, often within days. Blood pressure in the portal vein (the main vein bringing blood to the liver) climbs above 10 mmHg. This is portal hypertension. It’s the root of most complications. It forces blood to find new paths-through fragile veins in the esophagus and stomach. These veins swell into varices. And when they rupture? Bleeding. It’s sudden. It’s massive. And it kills 15-20% of people during the first episode. Even with treatment, half of those who survive will bleed again within a year if nothing is done. Then there’s hepatic encephalopathy. Your liver normally filters toxins from the blood. When it fails, ammonia and other poisons build up. The brain gets foggy. People forget names. They get confused. They might slur their speech or act oddly. In severe cases, they slip into coma. About one in three decompensated cirrhosis patients will face this. It’s not just a neurological issue-it’s a social one. Many patients say they’ve lost jobs, friendships, even custody of children because of the brain fog. And then there’s cancer. Cirrhosis is the #1 risk factor for liver cancer. Between 2% and 8% of people with cirrhosis develop hepatocellular carcinoma every year. That’s not rare. That’s predictable. And if you’re not getting screened, you’re gambling with your life.How Doctors Measure How Bad It Is
Not all cirrhosis is the same. That’s why doctors use scoring systems to see where you stand. The Child-Pugh score looks at five things: bilirubin (a liver enzyme), albumin (a protein), INR (how fast your blood clots), ascites, and brain function. A score of 5-6 means you’re in Class A-your liver still works well. You have a 100% chance of surviving a year. Class C? Score of 10-15. Your survival drops to 45%. That’s not a guess. That’s data from 2022 AASLD guidelines. But the real game-changer is the MELD score. It’s based on three lab values: creatinine, bilirubin, and INR. A score under 10? Low risk. Over 15? You’re in danger. Over 20? Transplant should be on the table. Over 25? You’re on a countdown. MELD isn’t perfect. It doesn’t capture how bad your brain fog is or how often you’re hospitalized. But it’s what transplant centers use to decide who gets a liver next.The Complications-And How to Stop Them
Ascites: First step? Cut salt. Less than 2 grams a day. That’s harder than it sounds. A single slice of bread has 230mg. Most processed foods are loaded. Diuretics come next-spironolactone and furosemide. Most people respond. But 10% don’t. They need their belly drained. Large-volume paracentesis. Every time, they get albumin infused to keep blood pressure stable. Skip this, and 37% of patients crash into circulatory failure. With albumin? Down to 10%. Variceal bleeding: If you have large varices, you get a beta-blocker-nadolol or propranolol. These lower pressure in the portal vein. They cut bleeding risk by 45%. Carvedilol works even better, lowering pressure more. But they can’t be used if you have low blood pressure or asthma. Endoscopic banding is the go-to for active bleeding. After that, you need lifelong meds. Without them, 60% rebleed in a year. Hepatic encephalopathy: Lactulose is the first-line treatment. It pulls ammonia out through your bowels. But it causes diarrhea. A lot of people quit because of it. Rifaximin, an antibiotic that stays in the gut, reduces flares by 58% compared to placebo. It’s expensive-$1,200 a month without insurance-but it saves hospital visits. Some patients say it’s the only thing that lets them go out in public again. Hepatocellular carcinoma: Every six months, get an ultrasound. That’s it. No CT. No MRI. Just ultrasound. It finds tumors early-when they’re still small and curable. If you skip screening, you’re 70% more likely to be diagnosed at a stage where treatment won’t work.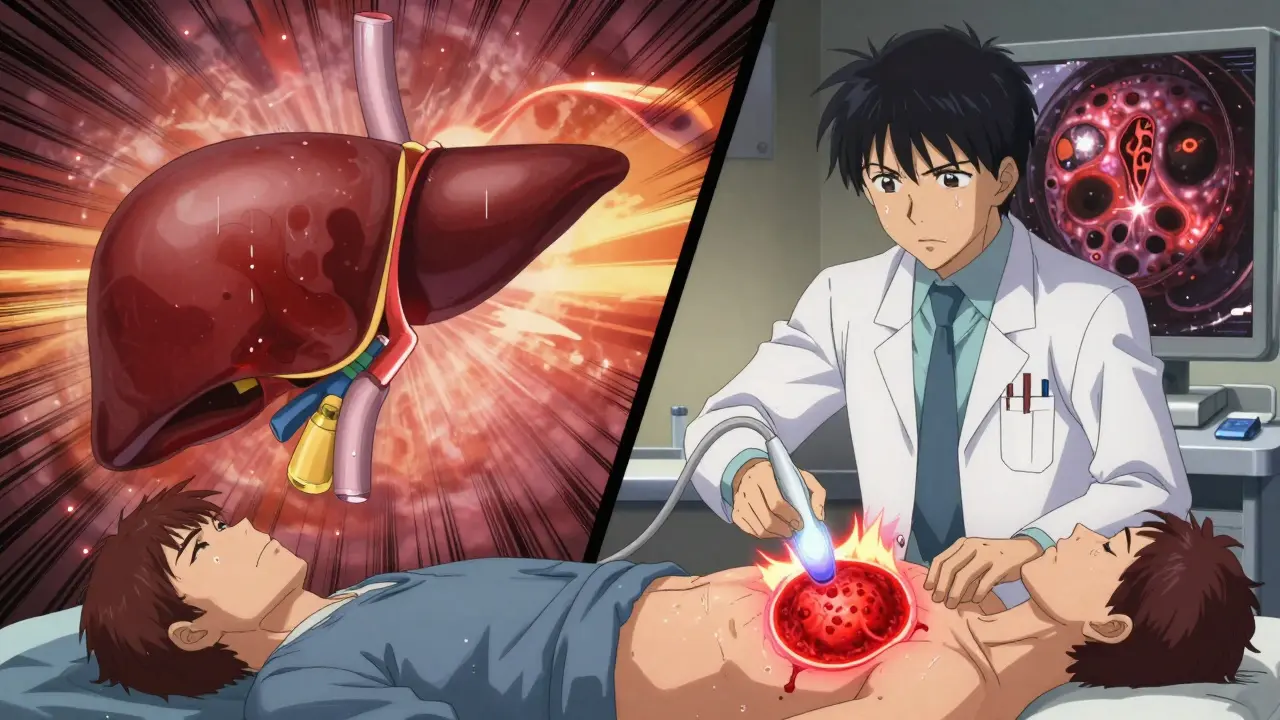
What Works-And What Doesn’t
The best treatment for cirrhosis? Stop the damage. If you drink, quit. If you have hepatitis C, get treated. Direct-acting antivirals cure over 95% of cases-even in cirrhosis. If you have fatty liver disease, lose weight. Even 5-10% of body weight can slow or reverse early scarring. But here’s the hard truth: once cirrhosis is advanced, you can’t undo it. You can only slow the fall. That’s why multidisciplinary care matters. A hepatologist alone can’t do it. You need a dietitian to help you eat under 2g of sodium. A social worker to help you navigate insurance and transplant lists. An addiction specialist if alcohol is the cause. A nurse practitioner who calls you weekly to check your weight and meds. One study found that structured care cut ER visits by 40% and improved medication adherence from 62% to 85%. That’s not a small win. That’s life or death.The New Hope-And the Real Limits
In March 2024, the FDA approved resmetirom (Rezdiffra) for MASH-related cirrhosis. It’s the first drug shown to reduce liver fibrosis in a phase 3 trial. In one year, 22.6% of patients had less scarring. It’s not a cure. But it’s a start. AI tools like CirrhoPredict are being tested. They use routine blood tests to predict who’s going to decompensate in the next 90 days-with 88% accuracy. Imagine if your doctor could call you before you got sick. Before you ended up in the hospital. That’s not science fiction anymore. Transplant remains the only cure. But the system is broken. In 2022, there were 11,346 people on the waiting list. Only 8,391 got a liver. Twelve percent of those waiting died in a year. New policies now try to factor in quality of life-not just MELD scores. Someone with severe encephalopathy might have a lower MELD than someone with just ascites. But their suffering? It’s worse.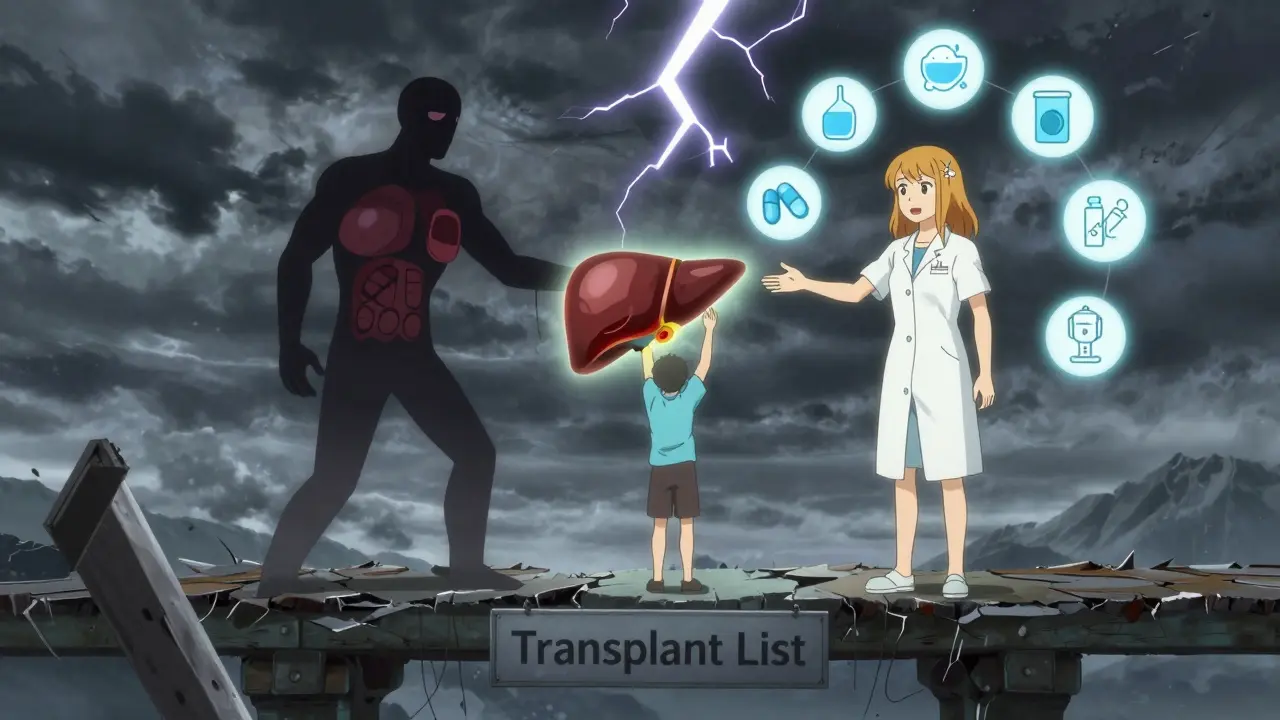
What Patients Really Live With
On Reddit, someone wrote: "I’ve missed 12 family events because lactulose diarrhea won’t stop." Another said: "I used to work full-time. Now I can’t get out of bed before noon." But then there’s this: "18 months post-transplant, my MELD score dropped from 28 to 9. I went back to work. I hugged my kids without being scared I’d collapse." The truth is, cirrhosis doesn’t just attack your liver. It attacks your dignity. Your independence. Your relationships. The medical system treats the labs. But patients are living with the fallout.What You Can Do Right Now
- If you have cirrhosis: Get screened for liver cancer every 6 months. No exceptions.
- If you have ascites: Weigh yourself daily. A 2-pound gain in one day? Call your doctor. That’s fluid building up.
- If you’re on beta-blockers: Don’t stop them unless your doctor says so. Stopping suddenly can cause bleeding.
- If you drink: Quit. No "cutting back." No "just weekends." You’ve already damaged your liver. More alcohol = faster death.
- If you have hepatitis C: Get treated. Even if you feel fine. The virus doesn’t care how you feel.
- If you’re on a transplant list: Keep your vaccinations up. Infections can kick you off the list.
Cirrhosis isn’t a death sentence. But it’s a wake-up call. The window to change things is narrow. Once you’re in decompensated cirrhosis, every month counts.