Every year, over 15 million people in the U.S. take medications that can silently destroy their hearing. Many never know it’s happening until it’s too late. The damage doesn’t come from loud music or aging - it comes from drugs meant to save lives: antibiotics, chemotherapy, even antidepressants. These are called ototoxic medications, and they target the tiny hair cells in your inner ear - cells that don’t grow back.
What Exactly Is Ototoxicity?
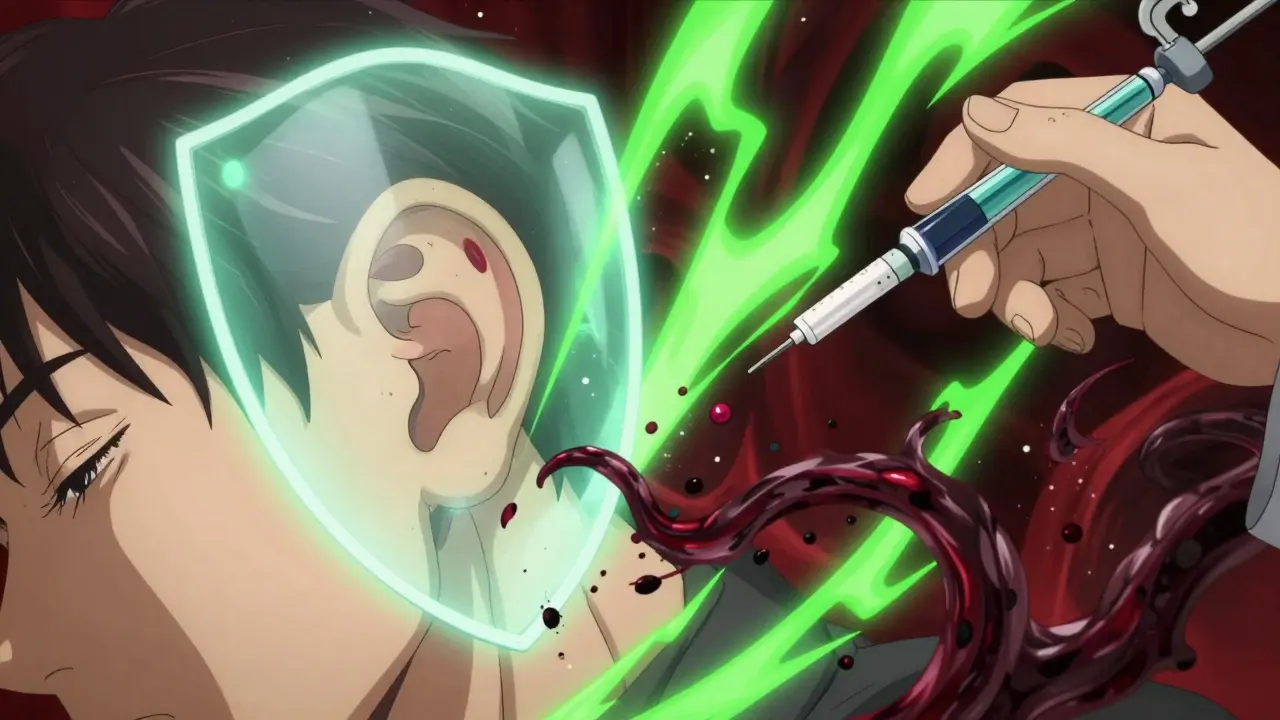
Ototoxicity means poison to the ear. It’s not just about volume. It’s about precision. The inner ear has over 15,000 hair cells that convert sound waves into electrical signals your brain understands. When ototoxic drugs enter the bloodstream, they can cross the blood-labyrinth barrier - a natural shield that normally protects the inner ear - and directly kill those cells. Once gone, they’re gone for good. This isn’t rare. Around 600 prescription drugs are known to carry this risk, according to the American Speech-Language-Hearing Association. The most dangerous ones are used daily in hospitals and clinics. Cisplatin, a chemotherapy drug for cancer, affects 30-60% of patients. Gentamicin, a common antibiotic for severe infections, causes permanent hearing loss in up to 63% of people on long-term treatment. These aren’t side effects you can ignore - they’re predictable, measurable, and often preventable.Which Medications Are the Biggest Threats?
Not all ototoxic drugs are created equal. Some hit hard and fast. Others creep in slowly. Here’s who’s most dangerous:- Aminoglycoside antibiotics: Gentamicin, tobramycin, amikacin, streptomycin. Used for drug-resistant infections like tuberculosis or sepsis. Hearing loss starts in the high frequencies - you might not notice until you can’t hear birds chirping or children’s voices clearly. Risk jumps sharply after seven days of use.
- Cisplatin: A cornerstone of cancer treatment for ovarian, lung, and testicular cancers. It doesn’t just damage hearing - it sticks around. Cisplatin builds up in the cochlea and keeps harming cells for months after treatment ends. About 18% of patients end up with severe or profound hearing loss.
- Carboplatin and oxaliplatin: These are cisplatin alternatives. Much safer. Carboplatin causes hearing loss in only 5-15% of patients. Oxaliplatin is even lower - under 5%. But they don’t work as well for all cancers, so doctors must choose carefully.
- High-dose aspirin and NSAIDs: Temporary ringing or muffled hearing can happen with very high doses, but it usually reverses when you stop taking them.
- Some antidepressants: Tricyclics like amitriptyline and SSRIs like sertraline (Zoloft) and fluoxetine (Prozac) have been linked to tinnitus and hearing changes in sensitive individuals.
What’s surprising? Vancomycin, another powerful antibiotic, has a much lower ototoxic risk - around 5-10% - compared to gentamicin. And loop diuretics like furosemide (Lasix) can cause temporary hearing loss, especially when combined with aminoglycosides. That combo is a red flag.
How Does the Damage Actually Happen?
It’s not one single mechanism. Different drugs attack in different ways:- Oxidative stress: Cisplatin and aminoglycosides flood the inner ear with free radicals. These unstable molecules tear apart cell membranes and DNA until the hair cells die.
- Reduced blood flow: Some drugs narrow blood vessels feeding the cochlea. Without oxygen and nutrients, hair cells starve.
- Direct toxicity: Aminoglycosides bind to ribosomes in hair cells and shut down protein production - essentially starving them from the inside.
- Neurotransmitter disruption: Certain drugs interfere with the chemical signals between hair cells and the auditory nerve, muddling sound before it even reaches the brain.
Damage usually starts at the top of the cochlea - the part that handles high frequencies (4,000-8,000 Hz). That’s why early signs include trouble hearing birds, alarms, or consonants like “s,” “sh,” and “th.” You might think you’re just not hearing well in noisy rooms. But it’s not your brain - it’s your ear.
Why Standard Hearing Tests Miss the Warning Signs
Most clinics test hearing up to 4,000 Hz. That’s the standard. But ototoxic damage begins above that - at 6,000, 8,000, even 12,000 Hz. That’s why patients often report: “I had no idea until I lost my hearing completely.” One Reddit user on r/Cancer shared their story after their third cisplatin cycle: “My audiologist only tested up to 4,000 Hz. I didn’t notice anything wrong. Then, after my fourth cycle, I couldn’t hear my daughter’s voice on the phone. The test showed a sudden drop at 6,000 Hz - gone.” Standard audiograms are useless for early detection. You need high-frequency audiometry - testing up to 12,000 Hz - to catch damage before it spreads to lower frequencies. That’s not routine. In fact, only 45% of U.S. cancer centers do it consistently.What Monitoring Actually Looks Like
Effective monitoring isn’t optional - it’s lifesaving. Here’s what it takes:- Baseline test: Before starting cisplatin or aminoglycosides, get a full audiogram including 8,000-12,000 Hz. This is your reference point.
- Regular follow-ups: For cisplatin, test after each cycle. For aminoglycosides, test after every 3-5 doses. Don’t wait for symptoms.
- Otoacoustic emissions (OAE): This non-invasive test measures sound produced by healthy hair cells. If the signal weakens, damage is already happening - even before you hear a difference. OAE catches problems 25% earlier than standard tests.
- Vestibular checks: Some ototoxic drugs also damage balance. If you feel dizzy, unsteady, or nauseous during treatment, mention it. Vestibular testing can detect early signs.
Studies show that patients who get this kind of monitoring are 30-50% less likely to develop severe hearing loss. That’s not a small win - it’s the difference between living independently and needing a hearing aid at 35.
Who’s at Highest Risk?
Some people are born with a ticking time bomb in their DNA. About 1 in 500 people carry a mitochondrial mutation - m.1555A>G or m.1494C>T - that makes them 100 times more likely to go deaf from a single dose of gentamicin. These mutations are rare, but devastating. Other high-risk groups:- Children receiving cisplatin - up to 35% develop language delays due to undiagnosed hearing loss
- People with pre-existing hearing loss
- Those with kidney disease - impaired kidneys can’t clear ototoxic drugs fast enough
- Patients on multiple ototoxic drugs at once - like cisplatin + furosemide
- Older adults - aging ears are more vulnerable
Genetic screening isn’t routine yet. But if you or a close relative had sudden hearing loss after antibiotics, talk to your doctor. It could save your child’s hearing.

What’s New in Prevention and Treatment
There’s real hope now. In November 2022, the FDA approved sodium thiosulfate (Pedmark) to protect children’s hearing during cisplatin treatment for liver cancer. In clinical trials, it cut hearing loss risk by 48%. It’s not a cure - it’s a shield. Researchers are also testing:- N-acetylcysteine: An antioxidant that may protect against aminoglycoside damage
- Hyperbaric oxygen therapy: Early studies suggest it helps restore oxygen to damaged cochlear tissue
- Smartphone apps: Scientists at Oregon Health & Science University are developing apps that use phone speakers and headphones to test high-frequency hearing at home. If it works, monitoring could become as easy as a weekly check-in.
These aren’t sci-fi ideas. They’re real, and they’re coming fast.
What You Can Do Right Now
If you’re prescribed a high-risk medication:- Ask: “Is this drug known to affect hearing?”
- Request a baseline audiogram that tests up to 12,000 Hz - not just 4,000 Hz.
- Ask if OAE testing is available.
- Keep a symptom journal: Tinnitus? Muffled sounds? Dizziness? Write it down. Share it with your doctor.
- Don’t assume your oncologist or infectious disease specialist knows the risks. Be your own advocate.
If you’re already on one of these drugs and notice changes - even mild ones - don’t wait. Get tested. Hearing loss from ototoxic drugs is permanent. But catching it early? That’s your chance to change the outcome.
Why This Matters Beyond Hearing
Hearing loss isn’t just about missing the phone ring. It’s about isolation. Depression. Falls. Cognitive decline. A 2023 study found that untreated hearing loss increases dementia risk by 50%. For kids, it’s language delays. For cancer survivors, it’s losing the sound of their child’s laugh. The economic cost? Over $1 billion a year in the U.S. for hearing aids, therapy, and lost work. But the human cost? Priceless.These medications save lives. But they shouldn’t steal your quality of life. With the right monitoring, we can have both.
Can ototoxic hearing loss be reversed?
No. Once the hair cells in your inner ear are destroyed by ototoxic drugs, they don’t regenerate. That’s why early detection is critical - you can’t restore lost hearing, but you can stop further damage. If caught early, doctors may reduce your dose, switch medications, or use protective agents like sodium thiosulfate.
Do all antibiotics cause hearing loss?
No. Only certain classes - primarily aminoglycosides like gentamicin, tobramycin, and amikacin. Common antibiotics like amoxicillin, azithromycin, and doxycycline are not ototoxic. Vancomycin has a low risk compared to aminoglycosides. Always ask your doctor which antibiotics carry hearing risks before starting treatment.
How often should I get my hearing tested if I’m on cisplatin?
You should have a baseline test before treatment starts. Then, get tested after every chemotherapy cycle. For cisplatin, testing should include frequencies up to 8,000-12,000 Hz, not just the standard 4,000 Hz. Some clinics test weekly during continuous infusion. Don’t wait for symptoms - damage can happen between cycles.
Can I use over-the-counter hearing aids if I lose hearing from medication?
OTC hearing aids can help with daily communication, but they don’t fix the underlying damage. They also can’t be properly programmed without a full audiogram. Always see an audiologist first. They can determine if you need custom hearing aids, assistive devices, or even cochlear implants. Self-fitting devices may not address the specific pattern of high-frequency loss common with ototoxicity.
Is there a genetic test for ototoxicity risk?
Yes. Two mitochondrial DNA mutations - m.1555A>G and m.1494C>T - make people extremely sensitive to aminoglycosides. Genetic testing is available, but it’s not routine. It’s recommended if you or a close family member had sudden hearing loss after antibiotics. Some hospitals offer screening for children before starting chemotherapy.
What should I do if I notice ringing in my ears during treatment?
Tinnitus is often the first sign of ototoxic damage. Don’t ignore it. Tell your doctor immediately. Request a high-frequency audiogram and OAE testing. In many cases, adjusting the drug dose or switching medications can prevent further loss. The earlier you act, the better your chances of preserving hearing.