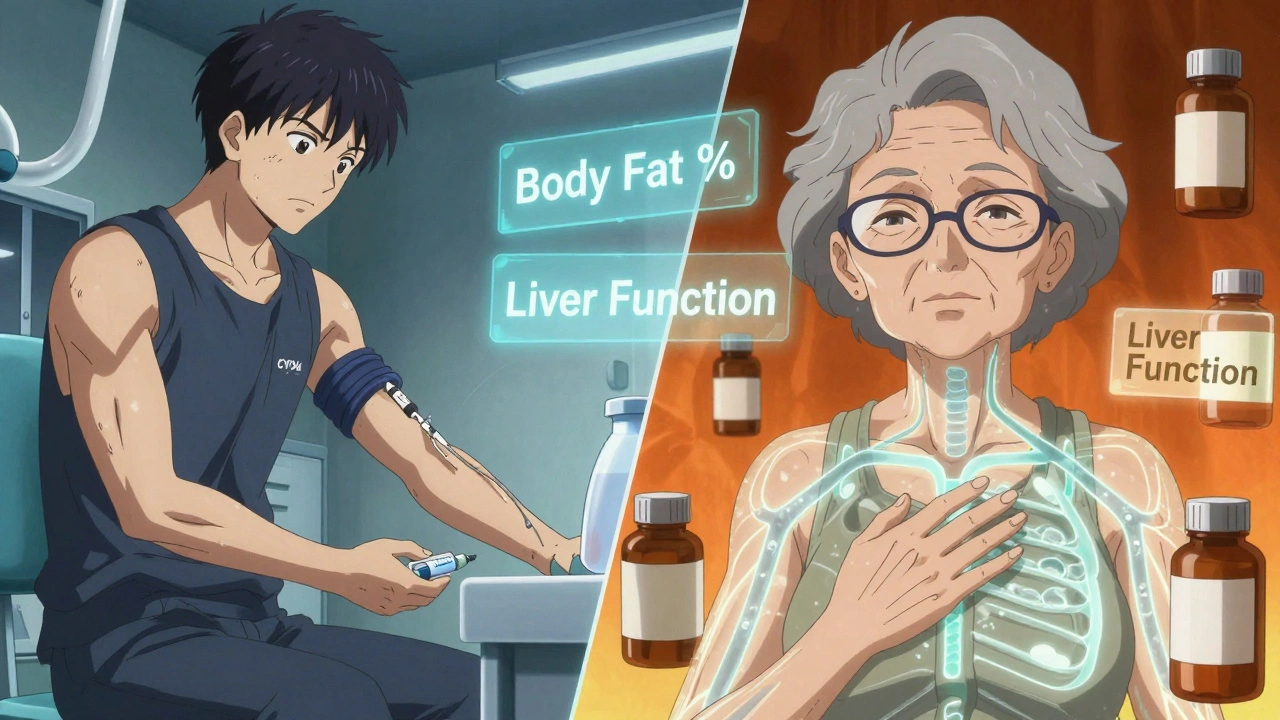
For decades, bioequivalence studies were done on young, healthy men - not because it made sense for everyone, but because it was easy. The assumption was simple: if a generic drug works the same in a 25-year-old male, it will work the same in a 65-year-old woman. But that’s not true. And today, regulators are forcing the industry to face that fact.
Why Bioequivalence Matters
Bioequivalence (BE) studies prove that a generic drug delivers the same amount of active ingredient into the bloodstream at the same rate as the brand-name version. If two drugs are bioequivalent, they’re considered therapeutically interchangeable. But that only holds if the study population reflects the real people who will take the drug. When BE studies skip women, older adults, or people with different body types, you’re not testing for safety or effectiveness across the population - you’re testing for a narrow slice of it.
Age Matters More Than You Think
As people age, their bodies change. Liver and kidney function slow down. Body fat increases. Stomach acid drops. These changes affect how drugs are absorbed, distributed, metabolized, and cleared. A drug that works fine in a 30-year-old might build up to toxic levels in a 70-year-old - or not work at all.
The FDA now requires that if a drug is meant for older adults, BE studies must include participants aged 60 or older. If they don’t, the sponsor must explain why. The EMA doesn’t mandate it, but they expect justification if elderly people are excluded. ANVISA in Brazil caps the upper age limit at 50 - a strict cutoff that doesn’t reflect real-world prescribing patterns for chronic conditions like hypertension or diabetes.
Here’s the problem: most BE studies still enroll people under 50. Why? Because it’s cheaper and faster. Older adults often have other health conditions, take multiple medications, or have lab values outside the "healthy" range. Excluding them makes recruitment easier. But it also means we’re approving generics for millions of elderly patients without ever testing them in that group.
Sex Differences Are Real - and They’re Being Ignored
Women aren’t just smaller men. Their bodies process drugs differently. Hormonal cycles affect absorption. Liver enzymes like CYP3A4 work at different rates. Body fat percentage is higher on average. All of this changes how drugs behave.
Take levothyroxine, a drug used by 63% women. Yet, in BE studies for this drug, women make up only 25% of participants on average. That’s not just a gap - it’s a blind spot. A 2018 study showed that in small BE trials (n=12), a few outliers in one sex could make it look like the generic wasn’t equivalent - even when it was. Larger studies (n=36) smoothed out those false signals. But many sponsors still run small trials to save money.
The FDA’s 2023 draft guidance says this clearly: if the drug is used by both sexes, you must include similar numbers of men and women. No more "it’s not necessary" excuses. The EMA is looser - they say subjects "could belong to either sex," but don’t require balance. That’s a dangerous loophole. A drug meant for both men and women shouldn’t be approved based on data from mostly men.
Regulatory Differences Around the World
Not all agencies are on the same page. Here’s how they stack up:
| Agency | Minimum Age | Maximum Age | Sex Requirement | Health Status |
|---|---|---|---|---|
| FDA (USA) | 18 | None (60+ encouraged) | ~50:50 unless justified | Healthy or stable chronic conditions |
| EMA (Europe) | 18 | None | Could be either sex - no balance required | Strictly healthy |
| ANVISA (Brazil) | 18 | 50 | Equal male/female distribution | Strictly healthy, non-smokers |
| Health Canada | 18 | 55 | No formal requirement | Healthy |
The FDA is the only one that explicitly ties sex representation to the target population. The EMA focuses on detecting formulation differences - not real-world use. ANVISA’s strict limits may seem rigid, but they force consistency. The result? A global patchwork. A generic drug approved in the U.S. might not meet Brazil’s standards - even if both countries claim to follow science.
Why This Isn’t Just About Fairness
This isn’t about political correctness. It’s about safety and effectiveness.
A 2017 study found a generic version of a blood pressure drug appeared bioinequivalent in men (79% absorption) but perfectly equivalent in women (95%). The difference? A tiny sample size. When the study was redone with 36 participants, the gap vanished. That’s the danger of small, unbalanced studies: they create false alarms - or worse, miss real problems.
Women report more adverse drug reactions than men. Why? Because we’ve been testing drugs on men and assuming the dose works for everyone. A 2023 University of Toronto study found that 37% of commonly tested drugs are cleared 15-22% faster in men than women. That means women might need higher doses to get the same effect - or they’re getting too much if the dose was set based on male data.
What Sponsors Are Doing - and What They Should Be Doing
Most sponsors still try to minimize costs. They pick young, healthy volunteers because they’re easier to recruit, have fewer medications interfering, and are less likely to drop out. But this is getting harder. The FDA now requires written justification for any deviation from balanced sex enrollment. That means sponsors must explain why they’re excluding women or older adults - and they need data to back it up.
Some are adapting. In 2022, 68% of contract research organizations (CROs) started actively recruiting women. They’re offering flexible hours, childcare support, and targeted outreach. But only 29% track sex-specific pharmacokinetics in their reports. That’s a missed opportunity. If you’re collecting data on men and women, you should analyze it separately. Otherwise, you’re just collecting numbers - not insights.

What’s Next? The Future of Bioequivalence
The FDA’s 2023 draft guidance is a turning point. It’s the first time a major regulator has made sex and age representation a hard requirement - not a suggestion. The EMA is reviewing its 2010 guidelines, and updates are expected in 2024. Brazil’s ANVISA already moved. It’s only a matter of time before others follow.
Future studies will likely need:
- Stratified randomization by sex and age group
- Pre-specified subgroup analyses in the study protocol
- Reporting of pharmacokinetic data by sex and decade of age
- Justifications for any exclusion - backed by published data
For narrow therapeutic index drugs - like warfarin or levothyroxine - regulators may soon require separate BE studies for men and women. Why? Because small differences in absorption can mean the difference between a clot and a bleed.
The goal isn’t to make studies bigger or more expensive. It’s to make them smarter. To stop pretending that a 25-year-old man is the default human. Real patients aren’t that simple. And the science is catching up.
Frequently Asked Questions
Why are bioequivalence studies usually done on young men?
Historically, researchers chose young, healthy men because they have fewer variables - no hormonal fluctuations, fewer medications, lower risk of pregnancy, and more consistent metabolism. It made studies easier to control and cheaper to run. But this practice ignored how real patients - especially women and older adults - process drugs. Regulatory agencies now require better representation because the old model doesn’t reflect reality.
Can a bioequivalence study include only women if the drug is meant for women?
Yes - but only if the drug is specifically intended for use by women only, such as certain hormonal therapies or drugs for female-specific conditions. The FDA allows single-sex studies in these cases. But for drugs used by both sexes - even if more common in women - the study must include both men and women in roughly equal numbers. Excluding men without justification can delay approval.
What happens if a BE study doesn’t include enough older adults?
If the drug is commonly used by older adults - like statins, blood pressure meds, or diabetes drugs - and the study excludes people over 60, the FDA will ask for a detailed justification. They may request additional studies in elderly populations before approving the generic. Skipping older adults risks approving a drug that’s unsafe or ineffective for the people who need it most.
Do I need separate bioequivalence studies for men and women?
Not always - but you need to analyze the data separately. A single study with balanced sex representation is usually sufficient. However, if the data shows a statistically significant difference in absorption between men and women, regulators may require further investigation. For drugs with a narrow therapeutic index, separate studies may eventually become standard.
Why is BMI so important in BE studies?
Body mass index affects how drugs are absorbed and distributed. Higher BMI can delay absorption, lower BMI can increase sensitivity to side effects. Agencies like the EMA and ANVISA set BMI limits (usually 18.5-30 kg/m²) to reduce variability. If participants are too overweight or underweight, their pharmacokinetics may not reflect the general population - making the study less reliable.
What This Means for Patients
You shouldn’t have to wonder whether your generic drug was tested on people like you. If you’re a woman over 60 taking levothyroxine, you deserve to know the generic version was studied in people who look like you - not just young men. The science is clear: one-size-fits-all doesn’t work in pharmacology. The regulatory shift isn’t about politics - it’s about making sure every pill you take is safe and effective for the person taking it.




